Blood Pressure Medication Timing Assistant
Determine if bedtime dosing is right for you
Based on your medication type and side effects, this tool helps you understand if taking your blood pressure medication at night could reduce daytime symptoms like dizziness and bathroom trips.
Select the primary type of blood pressure medication you're currently taking:
Often work better at night to reduce nighttime blood pressure
Generally beneficial for nighttime dosing
Mixed results; may cause nighttime swelling
Usually best taken in morning to avoid nighttime urination
Check any daytime side effects you experience:
How often do you wake up at night to use the bathroom?
Your Recommendation
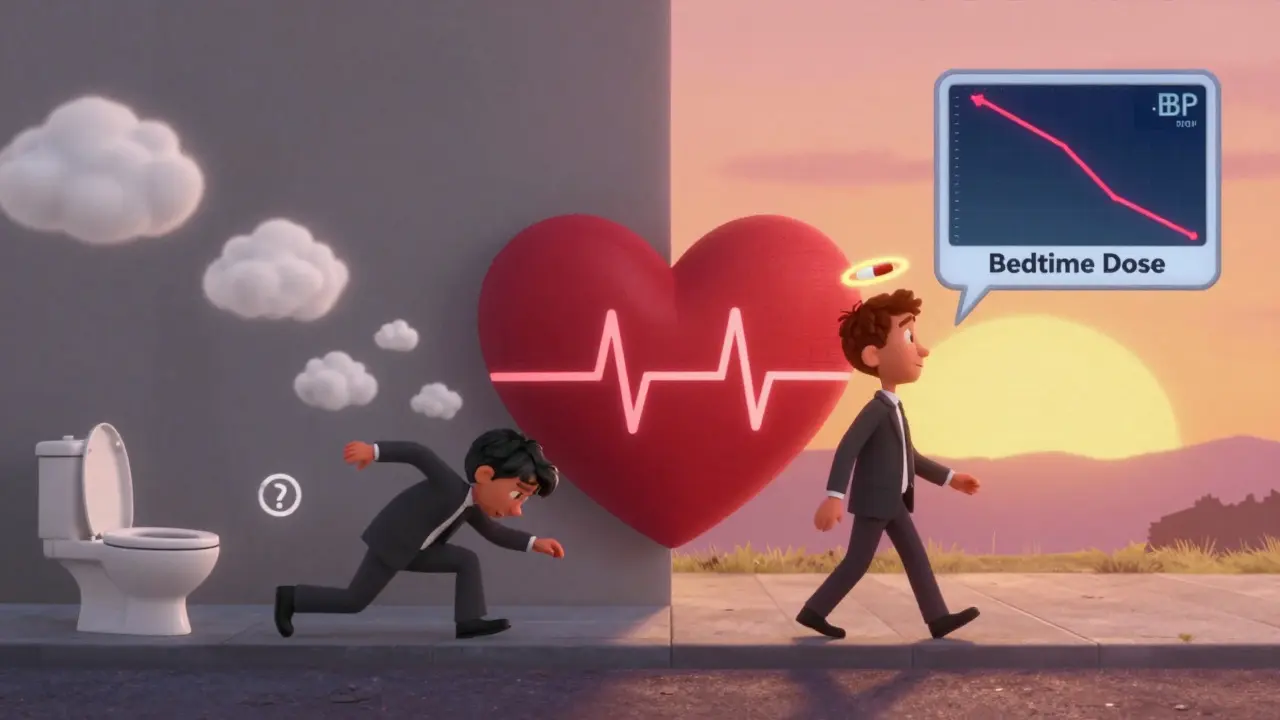
For millions of people taking blood pressure medication, the biggest problem isn’t the diagnosis-it’s the daytime side effects that make life harder. Morning dizziness. Frequent bathroom trips. Fatigue that ruins your workday. These aren’t just annoyances; they’re reasons people stop taking their pills. And when that happens, the real risk isn’t feeling lightheaded-it’s the heart attack or stroke you didn’t see coming.
Why Timing Matters More Than You Think
Your blood pressure doesn’t stay flat all day. It drops while you sleep, rises when you wake, peaks in the afternoon, and dips again at night. This rhythm isn’t just biology-it’s a warning sign. Studies show that your nighttime blood pressure is actually a better predictor of heart trouble than your daytime numbers. That’s why doctors are asking: What if we took our meds at night instead of morning? The idea sounds simple: take your pill before bed so the medicine works hardest while you’re sleeping. That way, you avoid the peak drug effect during your waking hours. And for some people, it works. But it’s not a magic switch. The science is messy. Some big studies say bedtime dosing cuts heart attacks. Others say it makes no difference. So what’s the real answer?What the Latest Research Really Shows
In 2024, two major Canadian trials-BedMed and BedMed-Frail-tracked over 4,000 people for nearly five years. They looked at falls, fractures, dizziness, cognitive decline, and even nighttime low blood pressure. The results? No clear safety advantage for bedtime dosing. In fact, frail older adults in nursing homes had just as many hypotensive episodes whether they took pills in the morning or at night. But here’s the twist: the morning group reported more dizziness and lightheadedness. That’s not a small detail. On Reddit, users like HypertensionWarrior87 shared how switching lisinopril to bedtime ended their morning dizziness that kept them out of work. Meanwhile, SeniorHealth45 had the opposite problem-nighttime leg swelling forced them back to morning dosing. The OMAN trial in China gave more clarity. People taking olmesartan-amlodipine at night didn’t get more dangerous drops in blood pressure overnight. No extra risk. No more fainting. Just the same control, just at a different time. And then there’s the bathroom issue. AAFP data showed 36.4% of bedtime takers had to get up at night versus 40% of morning takers. That’s not a huge difference-but for someone who’s already waking up twice a night, that 3.6% drop might mean the difference between a full night’s sleep and exhaustion.The Real Winner: Fewer Daytime Symptoms
The most consistent finding across studies isn’t about heart attacks or strokes. It’s about how you feel during the day. Cleveland Clinic’s analysis of the TIME study found that while fracture rates were the same, the morning dosing group had more dizziness. That’s huge. Dizziness is the #1 reason people quit their meds. If you’re too dizzy to walk the dog, drive to work, or stand in line at the grocery store, you’ll stop taking it-even if you know it’s important. A survey of 1,247 patients on the American Heart Association forum showed 78% of those with dizziness felt it within 2-4 hours after their morning dose. That’s not a coincidence. It’s the drug hitting its peak right when you’re trying to start your day. Switching to bedtime can shift that peak to when you’re asleep. You’re not awake to feel it. You wake up with your blood pressure already under control-not crashing or spiking.
Who Should Try Bedtime Dosing?
This isn’t for everyone. But if you have any of these, bedtime dosing might help:- You get dizzy or lightheaded within a few hours of taking your morning pill
- You’re constantly rushing to the bathroom during work hours
- You’ve been told you have “non-dipping” blood pressure-meaning it doesn’t drop enough at night
- You’ve tried other meds and side effects keep pushing you to quit
Who Should Avoid It?
Bedtime dosing isn’t risk-free. Avoid it if:- You already wake up multiple times at night to pee (nocturia)
- You have kidney disease or heart failure-your body may struggle to handle fluid shifts overnight
- You’re on diuretics like furosemide or hydrochlorothiazide-these can cause too much nighttime urination
- You have low blood pressure at night already (below 110/70)
What Your Doctor Should Be Asking You
Most doctors still default to morning dosing. It’s tradition. But that’s changing. A June 2024 survey found 43% of U.S. primary care doctors now bring up dosing timing with new patients-up from 28% in 2022. And 67% of those doctors say they sometimes recommend bedtime dosing specifically to reduce daytime side effects. Don’t wait for them to bring it up. Ask:- “Could taking this at night help with my dizziness?”
- “Is there a version of this pill that lasts longer overnight?”
- “Would my type of medication work better at night?”
What to Do Right Now
You don’t need to wait for a trial result. Here’s your action plan:- Track your side effects for a week. Note when you feel dizzy, tired, or need the bathroom.
- Check your pill label. Does it say “take in the morning”? That’s a suggestion, not a rule.
- Call your pharmacist. Ask: “Can I take this at night instead?” They know the drug’s half-life and peak timing.
- If you’re on a diuretic, don’t switch to night without talking to your doctor.
- Try taking your next dose at bedtime. Give it 3-5 days. Notice how you feel in the morning.
- If dizziness drops and sleep isn’t ruined, keep it. If not, go back to morning.
It’s Not About the Clock-It’s About Your Life
The biggest study ever on this topic, the TIME trial, found no difference in heart attacks or strokes between morning and bedtime dosing. That’s important. But it’s not the whole story. Medication adherence is the silent killer in hypertension. Half of all patients stop taking their pills within a year. Why? Side effects. Dizziness. Fatigue. Bathroom trips. These aren’t side notes-they’re the reason people die. If taking your pill at night means you can walk to the bus without holding onto a railing, or finish your shift without needing to nap, then that’s the win. You don’t need a 61% drop in heart events to justify it. You just need to feel like yourself again. The science may not be settled. But your life? That’s settled. You deserve to feel good while you’re alive-not just survive long enough to see the next study.Can I switch my blood pressure pill from morning to bedtime on my own?
You can try switching your timing, but don’t change your dose or stop the medication. Most blood pressure pills are safe to take at night, but some-like diuretics-shouldn’t be. Always check with your pharmacist or doctor first. Start by taking your next dose at bedtime and monitor how you feel over the next few days.
Will taking my blood pressure medicine at night cause me to wake up too often to pee?
It can, especially if you’re on a diuretic like hydrochlorothiazide. About 36% of people taking meds at night report nighttime urination, compared to 40% who take them in the morning. But if you’re already waking up multiple times, switching to night might make it worse. If you’re not on a diuretic, nighttime urination is rare. Talk to your doctor about your specific drug.
Does bedtime dosing lower blood pressure too much at night?
Studies like OMAN and BedMed-Frail found no increase in dangerously low nighttime blood pressure with bedtime dosing. In fact, for people whose blood pressure doesn’t drop at night (called non-dippers), bedtime dosing may help normalize the rhythm-which is actually protective. Your doctor can check your nighttime pressure with a 24-hour monitor if they’re concerned.
What if I forget to take my pill at night?
If you miss a bedtime dose, don’t double up in the morning. Just skip it and take your next dose at the regular time. Missing one dose won’t hurt you, but taking too much can cause dangerous drops in blood pressure. The key is consistency-not perfection. If you keep forgetting at night, morning might be better for you.
Do all blood pressure medications work the same at night?
No. ACE inhibitors (like lisinopril) and ARBs (like losartan) often work better at night because they help reduce nighttime blood pressure and protect the kidneys. Calcium channel blockers like amlodipine can cause leg swelling at night in some people. Diuretics should almost always be taken in the morning to avoid nighttime bathroom trips. Your drug matters as much as the time.

