Blood Thinner & Cosmetic Procedure Risk Calculator
Before You Start
This calculator is for informational purposes only. Always consult your prescribing doctor before changing any medications.
The risk of stopping anticoagulants can be greater than the risk of bleeding during the procedure. The correct decision depends on your individual health situation.
Your Results
Why Your Blood Thinners Matter More Than You Think Before a Cosmetic Procedure
If you’re on blood thinners - whether it’s aspirin, warfarin, or one of the newer DOACs like rivaroxaban or apixaban - and you’re thinking about getting a cosmetic procedure, you’re not alone. In fact, 25 to 40% of people going into dermatology or facial plastic surgery clinics are already taking these medications. It’s not just about aging. It’s about heart health, stroke prevention, and managing blood clots. But here’s the problem: most people assume they need to stop their meds before a laser treatment, filler injection, or even a simple mole removal. That’s not just outdated - it can be dangerous.
The old rule used to be simple: stop everything two weeks before surgery. But that was based on general surgery practices from the 1980s. Today, we know better. Stopping your blood thinner can actually put you at higher risk for a stroke or pulmonary embolism than the procedure itself does for bleeding. A 2014 survey of over 160 Mohs surgeons found 46 serious clotting events after patients stopped their meds - including 3 deaths and 24 strokes. And 54% of those happened after warfarin was stopped. That’s not a risk worth taking.
Not All Blood Thinners Are the Same
When doctors talk about "blood thinners," they’re lumping together very different drugs. The three main types behave in completely different ways:
- Antiplatelets like aspirin and clopidogrel make platelets less sticky. They’re often taken daily for heart disease or after stents.
- Warfarin is an older drug that blocks vitamin K. It needs regular blood tests (INR) to make sure it’s in the right range.
- DOACs - direct oral anticoagulants - include apixaban, rivaroxaban, dabigatran, and edoxaban. They work faster, leave your body quicker, and don’t need routine blood monitoring.
Here’s the key takeaway: aspirin and clopidogrel show almost no increase in bleeding risk for minor cosmetic procedures. Multiple studies confirm this. You can keep taking them. No need to stop.
Warfarin is trickier. If your INR is below 3.5 - which is the standard target for most people on it - you can usually proceed with most procedures without stopping. But if your INR is higher, the risk of bruising and bleeding goes up sharply. In one study, people on warfarin were 3.8 times more likely to have bleeding complications during facial surgery than those not on it.
DOACs fall somewhere in between. They’re safer than warfarin but still carry a small bleeding risk. A 2023 review found that when DOACs were continued during skin procedures, bleeding occurred in about 1.74% of cases. That’s low. And here’s the twist: when DOACs were stopped, the bleeding rate was actually higher in some studies - not lower. Why? Because stopping them can trigger rebound clotting, which leads to more inflammation and worse healing.
What Kind of Procedure Are You Getting?
Not every cosmetic procedure carries the same bleeding risk. You can’t treat a lip filler the same way you treat a facelift.
Low-risk procedures include:
- Laser treatments (fractional, IPL, CO2)
- Chemical peels
- Shave biopsies
- Excisions under 2 cm
- Fillers (lip, cheeks, tear troughs)
- Botox injections
For these, current guidelines from the British Society of Dermatologists (2023) say: continue all anticoagulants. No interruption needed. The chance of a serious bleed is less than 2%. The risk of stopping - a stroke, heart attack, or pulmonary embolism - is far greater.
Moderate-risk procedures include:
- Neck lifts
- Minor eyelid surgery (blepharoplasty)
- Some rhinoplasty procedures
- Large excisions or skin grafts
For these, DOACs can be held the morning of the procedure. Warfarin should be checked with an INR test the day before. If it’s under 3.5, proceed. Aspirin? Keep taking it.
High-risk procedures include:
- Full facelifts
- Complex rhinoplasty
- Body contouring with extensive tissue manipulation
- Flap reconstructions
These involve major blood vessels and large areas of tissue. Here, your surgeon may ask you to stop DOACs 24-48 hours before surgery. Warfarin might be stopped 5 days out, with bridging considered only in rare cases (like mechanical heart valves). But even here, bridging with heparin is generally not recommended - it increases bleeding without reducing clot risk.
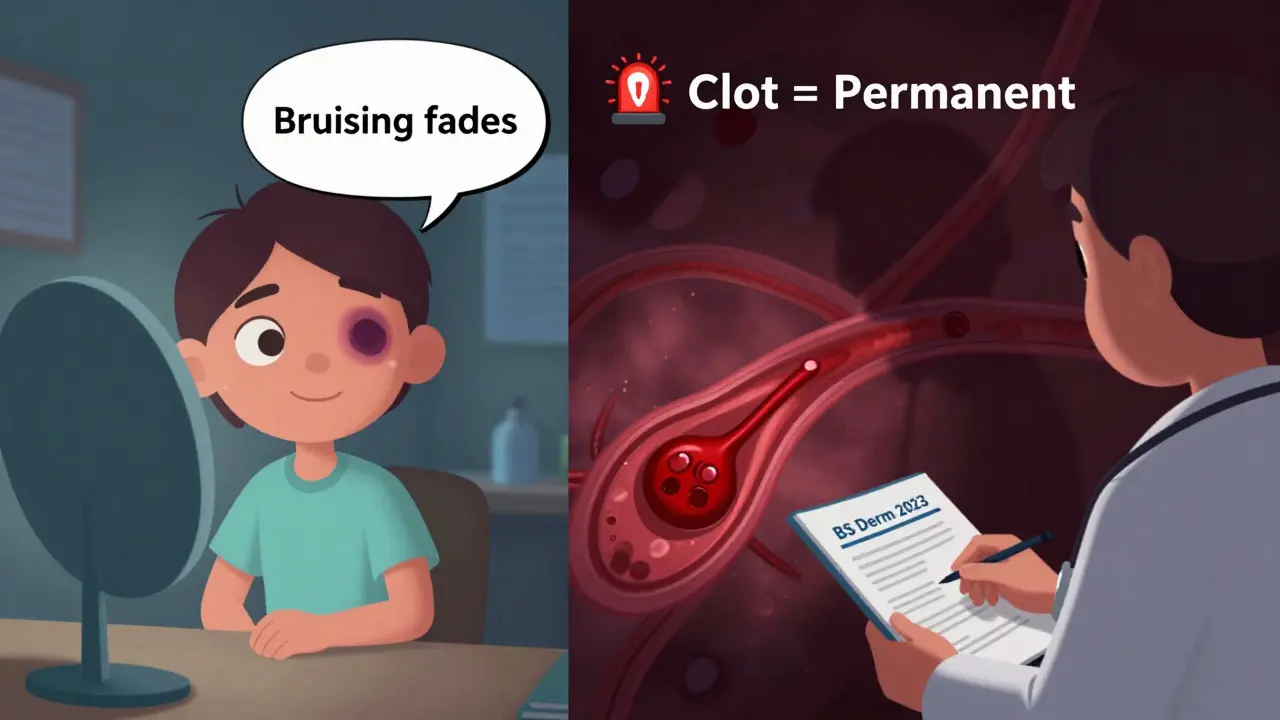
The Real Danger Isn’t Bruising - It’s the Clot
People worry about bruising. They see a purple mark under their eye after a filler and think, "I should’ve stopped my blood thinner." But here’s what they don’t tell you: bruising is cosmetic. A clot can kill you.
When you stop a DOAC or warfarin, your blood doesn’t just go back to normal. It goes into a hypercoagulable state - meaning it’s more likely to form clots. That’s why stopping aspirin for a few days can lead to a heart attack in someone with coronary disease. Stopping warfarin can cause a stroke in someone with atrial fibrillation.
A 2023 review found that even when anticoagulants are continued, the baseline risk of a clot is already low - between 0.6% and 1.1%. But when you stop them, that risk jumps to 0.15% on average for every procedure. That might sound small, but multiply that by the 17.7 million cosmetic procedures done in the U.S. in 2022. That’s hundreds of preventable strokes and deaths.
And bruising? It fades. It’s temporary. It’s uncomfortable, sure - but it doesn’t require a trip to the ER. A clot? That’s a life-altering event.
What Your Doctor Should Be Asking You
Too often, patients are told to stop their meds without a full discussion. Here’s what a good provider should do before your procedure:
- Ask exactly which medication you’re on - not just "blood thinner." Know the name and dose.
- Check your INR if you’re on warfarin - and make sure it’s below 3.5.
- Know your medical history: Do you have atrial fibrillation? A mechanical valve? A history of DVT or PE?
- Know the procedure’s bleeding risk - low, moderate, or high.
- Don’t assume you need to stop. Ask: "What’s the risk if I keep taking it?"
If your provider says, "Just stop everything," walk out. That’s not modern care. That’s old-school thinking.
For patients on dual therapy - say, aspirin plus clopidogrel - the risk is higher. Guidelines suggest delaying non-urgent procedures until you’re on monotherapy, if possible. But even then, stopping isn’t always the answer. Sometimes, it’s better to proceed with extra care: pressure, cautery, and meticulous technique.

What to Do Right Now
Don’t wait until the day before your appointment. Here’s your action plan:
- Write down every medication you take - including supplements like fish oil, ginkgo, or garlic pills. They can thin your blood too.
- Call your prescribing doctor (cardiologist, neurologist, GP) and ask: "Is it safe to continue my blood thinner for a cosmetic procedure?" Get their advice in writing.
- Bring that advice to your cosmetic provider. Don’t assume they know your full history.
- Don’t stop anything on your own. Even for a few days.
- Ask for a copy of the latest guidelines - like the British Society of Dermatologists’ 2023 update. It’s public. Your provider should be familiar with it.
And if you’re told you need to stop your meds for a filler or laser? Ask: "What’s the evidence for that?" If they can’t point to a recent study or guideline, you’ve got a red flag.
Bottom Line: Stay on Your Meds - Unless Your Doctor Says Otherwise
For most people, continuing anticoagulants during cosmetic procedures is not just safe - it’s the smarter, safer choice. The risk of bleeding is low. The risk of stopping is high. Bruising is annoying. A stroke is permanent.
The days of blanket discontinuation are over. Today’s standard is risk-stratified care: match the medication, the procedure, and your personal health history. And if your provider doesn’t do that? Find one who does.
It’s not about avoiding risks. It’s about managing them wisely.
Should I stop aspirin before a filler injection?
No. Multiple studies show aspirin does not increase bleeding risk in minor cosmetic procedures like fillers, Botox, or laser treatments. Stopping aspirin can raise your risk of a heart attack or stroke, especially if you’re taking it for cardiovascular reasons. Continue taking it unless your prescribing doctor advises otherwise.
Is it safe to get a facelift while on warfarin?
It can be, but only if your INR is below 3.5. Warfarin increases bleeding risk during major procedures like facelifts, and studies show patients on it are nearly four times more likely to have complications. Your surgeon will likely check your INR the day before and may ask you to stop warfarin 5 days prior if your INR is high or if you’re at high risk for clots. Never stop warfarin without consulting your cardiologist or prescribing doctor.
Can I keep taking apixaban before a rhinoplasty?
For a standard rhinoplasty (moderate-risk procedure), most guidelines recommend holding your morning dose of apixaban on the day of surgery. You can resume it 24 hours after the procedure, once bleeding risk has decreased. Do not stop apixaban for several days unless you have a very high clotting risk - and even then, bridging with heparin is rarely needed and often more dangerous.
Do I need to stop fish oil or vitamin E before a cosmetic procedure?
Yes. While not prescription drugs, supplements like fish oil, vitamin E, garlic, ginkgo biloba, and ginger can increase bleeding risk. Most surgeons recommend stopping these 7-10 days before any procedure involving cutting or laser. Unlike prescription anticoagulants, these aren’t monitored, so it’s safer to pause them. Always tell your provider about every supplement you take.
What if I’ve had a blood clot in the past? Can I still get cosmetic surgery?
Yes, but you need a careful plan. If you’ve had a deep vein thrombosis (DVT) or pulmonary embolism (PE), your doctor may keep you on anticoagulants long-term. The goal is to balance clot prevention with bleeding risk during surgery. For low-risk procedures, continue your meds. For higher-risk ones, your care team will coordinate between your hematologist and surgeon to determine if temporary interruption or bridging is necessary - but bridging is rarely recommended and only in extreme cases.


That's the entire thesis in one sentence.