Many people take fiber supplements to help with digestion, lower cholesterol, or manage blood sugar. But if you're also on medication, you could be putting your treatment at risk. Fiber doesn’t just pass through your body-it can grab onto drugs and carry them out before they’re absorbed. This isn’t a myth. It’s backed by real studies and clinical guidelines from Harvard, Mayo Clinic, and WebMD.
Why Fiber Interferes with Medicines
Fiber supplements like psyllium (Metamucil), methylcellulose (Citrucel), or oat bran don’t break down in your gut. Instead, they swell up, trap water, and move things along faster. That’s great for regularity. But when a pill and a fiber capsule are in your stomach at the same time, the fiber can bind to the drug. Think of it like a sponge soaking up a liquid. The drug sticks to the fiber, gets swept into the colon, and gets flushed out instead of entering your bloodstream. This isn’t the same as eating an apple or a bowl of oatmeal. Whole foods have fiber mixed with other nutrients, and the amount is spread out. Supplements? They pack in concentrated doses-sometimes 5 to 10 grams in one serving. That’s enough to mess with how your body handles certain drugs.Which Medications Are Most at Risk?
Not all drugs are affected equally. Some are highly sensitive. Others? Not so much. Here are the ones you need to be careful with:- Levothyroxine (for hypothyroidism): Multiple studies show fiber reduces how much of this drug gets absorbed. One study found patients had up to a 58% increase in LDL cholesterol because their thyroid meds weren’t working right.
- Metformin (for type 2 diabetes): Fiber can delay or reduce absorption, which might make your blood sugar harder to control.
- Lithium (for bipolar disorder): Even small changes in absorption can lead to toxicity or reduced effectiveness.
- Olanzapine (an antipsychotic): Fiber may lower blood levels, making the drug less effective.
- Carbamazepine (for seizures and nerve pain): Studies suggest fiber can reduce its absorption by up to 30% if taken together.
- Some antibiotics (like tetracycline or ciprofloxacin): Fiber can bind to them, especially if taken on an empty stomach.
On the flip side, drugs like rosuvastatin (Crestor) or clopidogrel (Plavix) don’t seem to be affected much-even with fiber supplements. But since we don’t know for sure about every drug, it’s safer to assume interference unless proven otherwise.
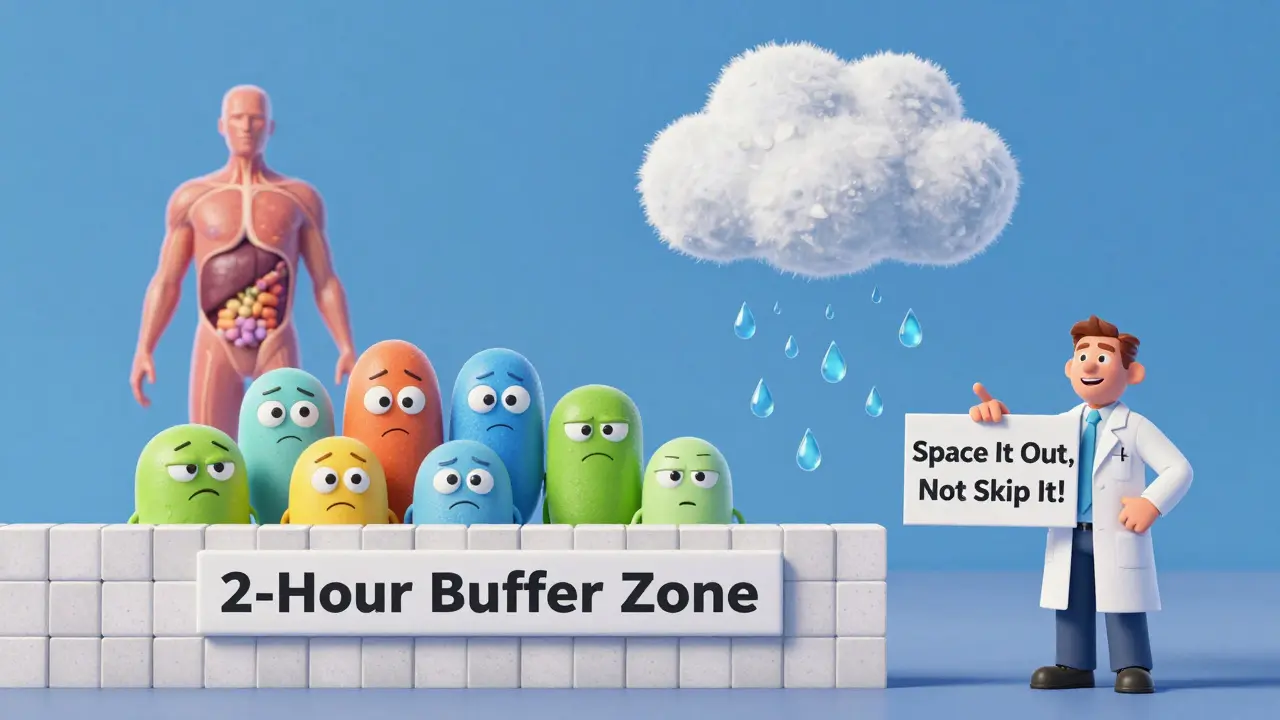
How Far Apart Should You Take Them?
This is the key. You can’t just avoid fiber. You need to time it right.Harvard Health, WebMD, and Mayo Clinic all agree: take your fiber supplement at least 2 to 3 hours before or after your medication.
Some sources go further. FreeRX recommends 4 hours apart for lithium, metformin, and olanzapine. Why? Because these drugs have a narrow therapeutic window-meaning even a small drop in absorption can cause real problems.
Here’s a simple rule to follow:
- If you take your medication in the morning, wait until at least 11 a.m. to take your fiber supplement.
- If you take your fiber at night, take your medication before 7 p.m.
- Never take them together, even if you’re drinking water.
And don’t forget: fiber supplements need water. Always take them with at least 8 ounces (240 ml) of water. Otherwise, they can swell in your throat and cause choking. That’s not just a warning-it’s a real risk.

What About Fiber from Food?
Eating a salad with lunch or having bran cereal in the morning? That’s fine. You don’t need to time meals around your meds the same way.Why? Because food fiber is diluted. A banana has 3 grams. A cup of oats has 4. A serving of fiber supplement? 5 to 10 grams, all at once. Your body handles small, natural amounts differently. But if you’re eating a huge bowl of high-fiber food-say, 20 grams of fiber in one meal-it’s worth spacing out your meds by a couple of hours.
What If You Already Took Them Together?
If you accidentally took your fiber and medication at the same time, don’t panic. One mistake won’t ruin your treatment. But if it happens often, it could lower your drug levels enough to cause symptoms.For example:
- If you take levothyroxine and fiber together daily, you might start feeling tired, gaining weight, or getting cold easily-even if your dose seems right.
- If you’re on metformin and your blood sugar starts creeping up, fiber timing could be the culprit.
Track your symptoms. Talk to your doctor. They can check your drug levels (like TSH for thyroid meds or HbA1c for diabetes) and adjust your plan.
Practical Tips to Stay on Track
Managing this isn’t hard. It just needs routine. Here’s how to make it stick:- Set phone alarms. One for your med, one for your fiber, 3 hours apart.
- Use a pill organizer. Put meds on one side, fiber on the other. No mixing.
- Don’t take fiber at bedtime. It can cause bloating, gas, or cramps that disrupt sleep. Take it earlier in the day.
- Read labels. Some fiber supplements say on the bottle: "Take at least 2 hours before or after other medications." Don’t ignore it.
- Ask your pharmacist. They know what’s in your prescription list. A quick check can save you from a hidden interaction.
Don’t Skip Fiber-Just Time It Right
The truth? Fiber saves lives. People who eat enough fiber have lower risks of heart disease, stroke, type 2 diabetes, and colon cancer. The average adult in the U.S. eats only 15 grams a day. The recommended amount? 21 grams for women over 50, 30 for men.Don’t quit your fiber supplement because you’re scared of interactions. Just move it. Space it out. Make it part of your routine. You can still get all the benefits-without risking your meds.
And if you’re unsure? Ask your doctor. Bring your supplement bottle. Show them your medication list. They’ll help you find the right balance. Because health isn’t about avoiding one thing-it’s about managing all of it together.
Can I take fiber and my medication at the same time if I drink a lot of water?
No. Drinking water helps fiber move safely through your system, but it doesn’t stop the drug from binding to the fiber. The interaction happens at a molecular level. Water won’t prevent it. Always separate them by at least 2 hours.
Is psyllium the worst fiber for drug interactions?
Psyllium (found in Metamucil) is one of the most studied and shows the clearest interference with drugs like levothyroxine and metformin. But other fibers-like oat bran, soy fiber, and methylcellulose-can also bind to medications. Don’t assume one is safer than another unless your doctor confirms it.
What if I take my fiber at night and my meds in the morning?
That’s actually a good setup-if you take your meds before 7 a.m. and fiber after 10 p.m., you’re safely spaced apart. The key is the 2-3 hour gap, not the time of day. Just make sure you’re not taking fiber right before bed if it causes bloating or gas.
Do fiber supplements affect blood pressure meds?
There’s no strong evidence that fiber interferes with most blood pressure medications like lisinopril, amlodipine, or hydrochlorothiazide. But because research is limited, it’s still safest to separate them by 2 hours. If you’re on multiple meds, check with your pharmacist.
Can I switch to a different fiber supplement to avoid interactions?
Switching fiber types won’t solve the problem. All fiber supplements-whether soluble or insoluble-can interfere with drug absorption. The issue isn’t the type of fiber. It’s the concentrated dose. The solution is timing, not substitution.



Just started taking psyllium last week and didn't realize it could mess with my metformin. Thanks for the heads up. I've been spacing them out now and my blood sugar's actually been more stable. Small change, big difference.
Set two alarms. One for meds. One for fiber. Works every time.
People really dont read labels do they I mean the bottle says right on it take 2 hours apart but somehow everyone thinks they know better than science I mean its not rocket science its just timing
I used to take my fiber at night because I thought it would help me sleep better, but then I started having crazy bloating and restless nights. After reading this, I switched to taking it right after lunch, and wow. What a difference. My digestion improved, my energy didn't crash, and I finally stopped waking up feeling like I'd eaten a brick. Also, my thyroid levels stabilized after I stopped mixing it with levothyroxine. I didn't even realize that was the issue until I saw this post. Seriously, people need to stop treating supplements like candy. They're not harmless. They're powerful.
Bro I took fiber with my pills for 6 months and thought I was fine. Turns out my BP was spiking because of it. Now I wait 3 hours. Life changed.
So you're telling me I can't just chow down my Metamucil with my lithium like it's a smoothie? 😅 I mean come on man, I'm not a robot. I'm just trying to feel human. But I guess if science says so... I'll do it. Still feels weird though. Like I'm being told how to breathe. 🤷♂️
In India we have been taking chia and psyllium with meals for centuries. No one dies. No one has issues. Why are you Westerners so scared of natural things? You overthink everything. Fiber is fiber. Medication is medication. If your body can't handle it, maybe your body is broken. Not the fiber.
LMAO so now we're treating fiber like a drug cartel? "You must wait 3 hours! You are not allowed to mix!" This is why America is falling apart. You turn every damn thing into a medical emergency. I eat oatmeal with my pills. I'm fine. My doctor says I'm fine. So why are you all panicking? You're the reason people hate healthcare.
Thank you for sharing this. I’ve been taking fiber with my meds for months because I forgot to separate them. It’s so easy to slip into that habit. I didn’t realize my fatigue and mood swings were linked to this. I just started spacing them out and already feel clearer-headed. It’s not about being perfect-it’s about being aware. Small changes, big impact.
OMG I JUST REALIZED I’VE BEEN TAKING MY METFORMIN AND METAMUCIL TOGETHER FOR A YEAR. MY BLOOD SUGAR HAS BEEN ALL OVER THE PLACE. I THOUGHT IT WAS STRESS OR SLEEP OR MY KID’S TEENAGE YEARS. NOPE. IT WAS THE FIBER. I’M CRYING. I’M SO STUPID. BUT ALSO SO GRATEFUL THIS POST EXISTED. I’M SETTING ALARMS RIGHT NOW. THANK YOU.
Just take it at night. Done.
Look, I get the science. But let’s be real - most people aren’t taking 10g of fiber in one go. They’re eating a banana, a bowl of oatmeal, and a few almonds. That’s not a supplement. That’s breakfast. The real issue here is pharmaceutical companies pushing fear to sell more tests, more labs, more alarms. We’re turning healthy habits into medical compliance drills. And honestly? It’s exhausting.
Yes, fiber can interfere. But so can coffee. So can grapefruit. So can sleeping in. We don’t panic about those. Why this? Because it’s easy to blame the supplement. Not the system. Not the timing of your work schedule. Not the fact that you have to take 7 pills at 7 different times because your doctor doesn’t coordinate.
I’m not saying ignore the advice. I’m saying: don’t let fear make you feel broken. You’re not failing because you forgot. You’re just human. Adjust. Learn. Move on. Don’t turn your life into a spreadsheet.