Immunosuppressant Hair Loss Risk Calculator
Assess Your Risk
This calculator estimates your risk of hair loss based on the immunosuppressant medication you're taking and other factors mentioned in the article.
When you’re taking immunosuppressants to keep a transplanted organ alive or to control a serious autoimmune disease, the last thing you expect is to start losing your hair. Yet for many, it happens-often quietly, over months-and it can feel like a betrayal. You’re following every rule, taking your pills, surviving the illness or surgery-and now your hair is thinning, falling out in the shower, clinging to your brush. It’s not just cosmetic. It’s emotional. It’s identity. And it’s more common than most doctors admit.
Why Your Hair Is Falling Out (It’s Not Just Stress)
Not all hair loss is the same. Chemotherapy wipes out hair fast because it attacks rapidly dividing cells-including those in your hair follicles. That’s anagen effluvium. But immunosuppressants? They don’t work that way. Most cause telogen effluvium: a slow, diffuse shedding where hair follicles prematurely shift from growing to resting. Think of it like your scalp going into survival mode. Your body isn’t rejecting the drug-you’re just not growing hair like you used to.
This isn’t random. Drugs like tacrolimus (Prograf), mycophenolate (CellCept), and methotrexate interfere with the hair growth cycle by disrupting cellular signals needed for follicles to stay in the active phase. A 2003 study of kidney-pancreas transplant patients found that nearly 3 out of 10 developed noticeable hair loss on tacrolimus. And here’s the kicker: 11 of those 13 people were women. Gender matters. So does genetics. If you already have a family history of thinning hair, you’re more likely to see it worsen under these drugs.
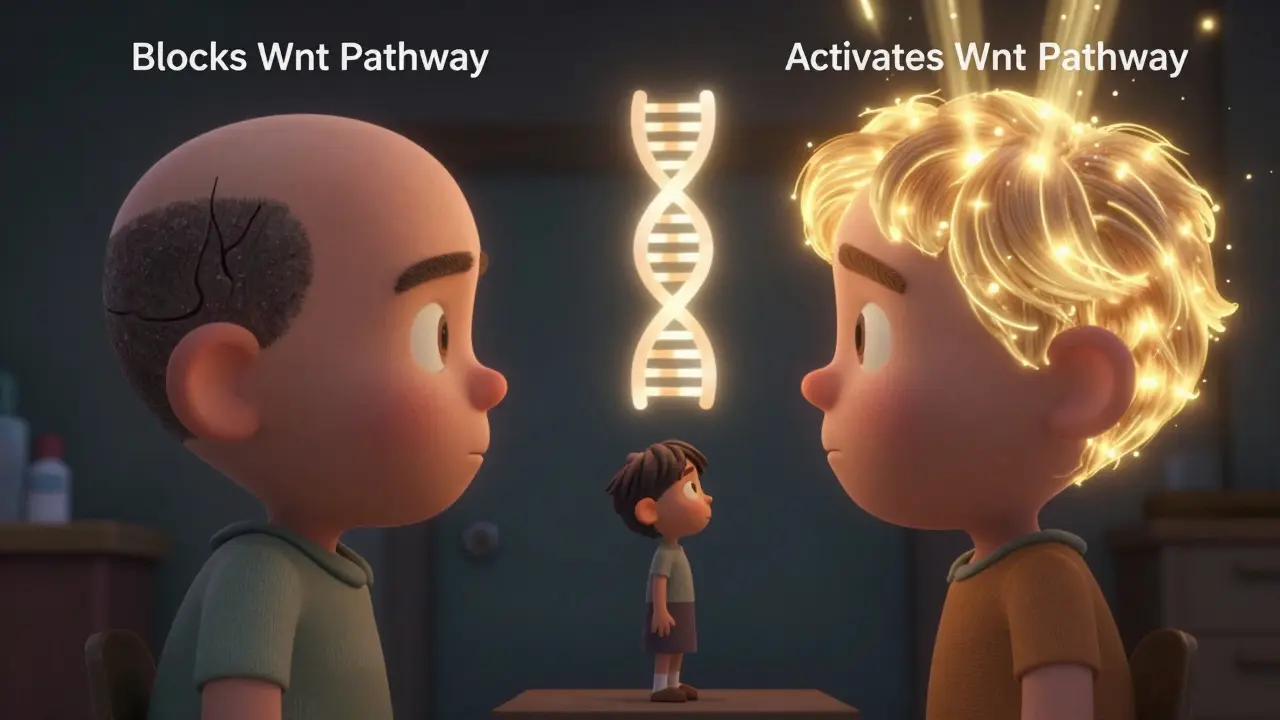
Not all immunosuppressants do this. Cyclosporine? It often does the opposite. Studies show 20-30% of people on cyclosporine develop unwanted facial or body hair. It activates Wnt pathways-same ones that help hair grow. Tacrolimus? It blocks them. Same class of drugs. Opposite effects. That’s why switching from tacrolimus to cyclosporine has helped some patients regrow their hair completely.
Which Medications Are Most Likely to Cause Hair Loss?
It’s not a level playing field. Some drugs carry a much higher risk than others. Here’s what the data shows:
- Tacrolimus: 28.9% of kidney-pancreas transplant patients experience hair loss. It’s the most common offender.
- Leflunomide (Arava): Around 10% of rheumatoid arthritis patients report noticeable thinning.
- Methotrexate: 3-7% of users, usually at higher doses. Often reversible with folic acid.
- Myophenolate mofetil: Around 5-8%, though less studied than tacrolimus.
- Etanercept (Enbrel): Only 4.4% report hair loss-lower than most traditional drugs.
- Cyclosporine: Rarely causes hair loss. Often causes extra hair growth.
It’s not just the drug-it’s the dose, how long you’ve been on it, and your body’s unique reaction. Hair loss usually shows up 3 to 6 months after starting the medication, but some people don’t notice it until a year in. The delay makes it easy to blame stress, hormones, or aging instead of the pill you’re taking daily.
Who’s Most at Risk?
If you’re a woman, you’re more likely to notice this side effect. The 2003 study showed an 11:2 female-to-male ratio in tacrolimus-related hair loss. Why? We don’t fully know. Hormones might play a role. So might how your body metabolizes the drug. But it’s also about perception. Women are more likely to notice changes in hair volume, and more likely to report it.
Other risk factors:
- Pre-existing androgenetic alopecia (family pattern baldness)
- High doses of medication
- Combining immunosuppressants with other hair-thinning drugs like beta-blockers or statins
- Autoimmune diseases that already cause hair loss-like lupus or alopecia areata. In these cases, it’s hard to tell if the drug or the disease is to blame.
One study from the Cleveland Clinic found that patients with autoimmune conditions already linked to hair loss had a 40% higher chance of severe shedding on immunosuppressants. That’s a double hit.
What Actually Helps? Real Strategies, Not Hype
You’ve probably heard about biotin, scalp massages, and expensive laser caps. Let’s cut through the noise. Here’s what works-and what doesn’t-based on real data and clinical experience.
1. Minoxidil (Rogaine)
This is the most studied and most recommended treatment. The American Academy of Dermatology supports using 5% minoxidil foam or solution twice daily. It doesn’t stop the drug from causing hair loss, but it helps follicles stay active longer. In the same 2003 study, 12 out of 13 patients using minoxidil saw improvement. One didn’t respond-and that person switched from tacrolimus to cyclosporine and regrew all their hair.
It takes time. Don’t expect results in 2 months. Most people see less shedding after 3-4 months. Visible regrowth? That’s 6-8 months. Stick with it. And don’t stop when you see progress. Stopping minoxidil means you’ll lose the new growth.
2. Switching Medications
If you’re on tacrolimus and losing hair, talk to your transplant team about switching to cyclosporine. Yes, cyclosporine has its own side effects-tremors, gum overgrowth, high blood pressure. But if hair loss is wrecking your mental health, it’s worth discussing. In clinical settings, this switch has resolved hair loss in patients who didn’t respond to minoxidil.
Don’t do this on your own. Stopping immunosuppressants without medical supervision can lead to organ rejection. One study found a 15.2% spike in rejection episodes among patients who cut their doses to avoid side effects.
3. Nutritional Support
Low zinc or biotin levels can worsen hair thinning. That doesn’t mean popping a supplement will fix everything-but correcting a deficiency helps. A 2022 meta-analysis found that 40-50% of people saw modest improvement with:
- Zinc: 50 mg per day (not more-too much can be toxic)
- Biotin: 10,000 mcg per day
- Vitamin D: Many transplant patients are deficient. Get your levels checked.
These won’t reverse drug-induced hair loss alone, but they support overall follicle health. Think of them as backup dancers, not the lead singer.
4. Low-Level Laser Therapy (LLLT)
Devices like Capillus82 or iRestore have been tested in small trials. One 2021 study with 120 participants showed a 22.3% increase in hair density after 26 weeks of using the device three times a week. It’s not magic, but for people who can’t use minoxidil (due to scalp irritation or pregnancy), it’s a solid option.
The Emotional Toll Nobody Talks About
One Reddit user, ‘KidneyWarrior42,’ wrote: ‘After 8 months on tacrolimus, I lost 40% of my hair. I stopped looking in mirrors.’
A Healthline survey of 587 people on immunosuppressants found that 78% said hair loss affected their social life. Nearly half admitted they’d thought about lowering their dose to stop it. That’s dangerous. But understandable.
Dr. Rodney Sinclair from the University of Melbourne says 22% of patients in one study considered quitting life-saving medication because of hair loss. That’s not just a side effect. It’s a crisis of adherence.
And it’s worse for women. Post-transplant, many already feel like their body has betrayed them. Losing hair adds shame. Avoiding photos. Wearing hats in summer. Feeling like you’re not yourself. This isn’t vanity. It’s mental health.
Some transplant centers now offer hair loss counseling as part of pre-transplant education. That’s new. In 2018, only 12% did. By 2023, it was 37%. Progress. But it’s still not standard everywhere.

What’s Coming Next?
Science is catching up. A 2023 clinical trial is testing topical JAK inhibitors-drugs already used for alopecia areata-for immunosuppressant-related hair loss. Early results look promising.
Another breakthrough? Genetic testing. Researchers found that people with a specific variation in the WNT10A gene are far more likely to lose hair on tacrolimus. Imagine being able to choose your immunosuppressant based on your DNA before you even start treatment. That’s not science fiction-it’s coming by 2025.
Scalp-cooling devices, once used only for chemo patients, are now being adapted for immunosuppressant users. Early trials show a 65% reduction in hair loss severity. It’s not widely available yet, but it’s coming.
What You Should Do Right Now
If you’re on an immunosuppressant and noticing hair thinning:
- Don’t panic. This is usually temporary and reversible.
- Don’t stop your medication. Talk to your doctor.
- Start minoxidil 5% twice daily. Give it 6 months.
- Get blood work: check zinc, vitamin D, ferritin, and thyroid levels.
- Ask if switching to cyclosporine is an option-especially if you’re female and on tacrolimus.
- Consider LLLT if minoxidil irritates your scalp.
- Seek support. Talk to others on forums like AARDA or r/transplant. You’re not alone.
Hair loss from immunosuppressants isn’t a sign you’re doing something wrong. It’s a biological side effect of staying alive. And with the right approach, most people get their hair back-or at least enough to feel like themselves again.
What You Should Never Do
- Never reduce your dose to stop hair loss. The risk of rejection or disease flare is real and deadly.
- Never blame yourself. This isn’t stress or poor diet. It’s the drug.
- Never wait until it’s severe to act. Early intervention means faster recovery.
Living with a transplanted organ or a chronic autoimmune disease is hard enough. You shouldn’t have to lose your hair on top of it. But with the right knowledge and support, you don’t have to.
Can immunosuppressants cause permanent hair loss?
No, hair loss from immunosuppressants is almost always temporary. Once the medication is stopped or switched, hair typically regrows within 6 to 12 months. The follicles aren’t destroyed-they’re just paused. The exception is if you have an underlying condition like scarring alopecia, which is rare.
Is hair loss from tacrolimus more common in women?
Yes. A major 2003 study found 11 out of 13 patients who lost hair on tacrolimus were women. While the exact reason isn’t fully understood, hormonal differences, genetic susceptibility, and possibly how women metabolize the drug likely play a role. Women are also more likely to notice and report thinning hair.
Will switching from tacrolimus to cyclosporine help my hair grow back?
In many cases, yes. Cyclosporine activates pathways that promote hair growth, while tacrolimus blocks them. Studies show patients who switched from tacrolimus to cyclosporine often saw full regrowth within 4-6 months. But cyclosporine has its own side effects, so this decision must be made with your transplant team.
How long does it take for hair to grow back after stopping the drug?
Hair regrowth usually begins 3-6 months after switching or reducing the medication. Full recovery can take 6-12 months. Using minoxidil during this time can speed up the process. Don’t expect results before 4 months-patience is key.
Can biotin or zinc supplements fix hair loss from immunosuppressants?
They can help, but they won’t fix it alone. If you’re deficient in zinc or biotin, correcting that can improve hair health and reduce shedding. But if the hair loss is caused by the drug, supplements won’t reverse it. Think of them as support, not a cure. Always check with your doctor before taking high doses.
Is there a blood test to predict if I’ll lose hair on immunosuppressants?
Not yet for routine use, but research is advancing. A 2023 study identified a genetic marker (WNT10A variant) that strongly predicts susceptibility to tacrolimus-induced hair loss. This could lead to personalized drug choices in the next few years, helping patients avoid medications likely to cause hair loss based on their DNA.
Should I see a dermatologist for this?
Yes, especially if you’re losing more than a handful of hairs daily or if it’s affecting your mental health. A dermatologist who specializes in hair disorders can confirm the cause, rule out other conditions, and recommend the right treatments-like minoxidil, LLLT, or even a medication switch. Many major transplant centers now have dermatologists on staff for this exact reason.


I didn't realize hair loss from these meds was so common. I've been on tacrolimus for three years and thought I was just getting older. Turns out it's the drug. Started minoxidil last month-slow progress, but I'm not panicking anymore.
My sister lost her hair on CellCept. She cried every time she brushed it. Switched to cyclosporine-hair grew back in five months. It’s not vanity, it’s survival.
they got you scared of your own body now dont they i mean why are we even taking these pills if they make you look like a ghost
I used to wear scarves everywhere. Not because of the cold, but because I couldn't face the mirror. I thought I was failing at being a survivor. Turns out, my scalp just needed a little nudge. Minoxidil didn't fix everything, but it gave me back the version of me that still recognized herself. That's worth every penny and every greasy pillowcase.
Man, I just wanna say-you’re not alone. I’m a kidney recipient from Nigeria, and I lost my curls on tacrolimus. Felt like I lost part of my identity. But I started minoxidil, got my zinc checked, and now I’m growing back what I lost. It’s slow, it’s messy, but it’s happening. You’re still you. The hair? Just a chapter, not the whole book.
the study says 3 out of 10 but they only looked at kidney pancreas patients what about liver or heart what about men what about people who dont have money for minoxidil
Thank you for the thorough and clinically grounded analysis. The distinction between telogen effluvium and anagen effluvium is critical for patient understanding. I appreciate the emphasis on evidence-based interventions over anecdotal remedies. This is precisely the kind of information that should be disseminated to transplant clinics globally.
so like... are we just lab rats for big pharma? they give us drugs to live but take our hair? and then sell us $80 foam to fix it? i mean... what even is life
It’s funny how we attach so much of our identity to hair. We think if we lose it, we lose our dignity, our femininity, our youth. But the truth is, the person who wakes up every morning and takes their pills, who shows up even when they feel like falling apart-that’s the real you. The hair is just the surface. It’s the courage beneath that matters. And if you’re reading this, you’ve already got it. You’re not broken. You’re just rearranging. And that’s okay. More than okay. It’s heroic.
Good info. I’m on mycophenolate and noticed thinning after 6 months. Started minoxidil. No magic, but less shedding. I didn’t know cyclosporine could help. Might ask my doc.
Just wanted to say-this post saved me. I was about to quit my meds because I couldn't stand looking in the mirror. Then I found this. Started minoxidil + LLLT. Hair’s coming back. Not full yet, but I’m not hiding anymore. 🙌
Thank you for including the emotional impact. Too often, this side effect is dismissed as trivial. It’s not. The shame, the isolation, the avoidance of social events-it’s real. I’m glad your post validates that.
It’s interesting how medicine focuses on survival, but forgets that living requires feeling like yourself. Hair isn’t just follicles-it’s memory, culture, self. Maybe the next frontier isn’t just better drugs, but better care for the whole person.