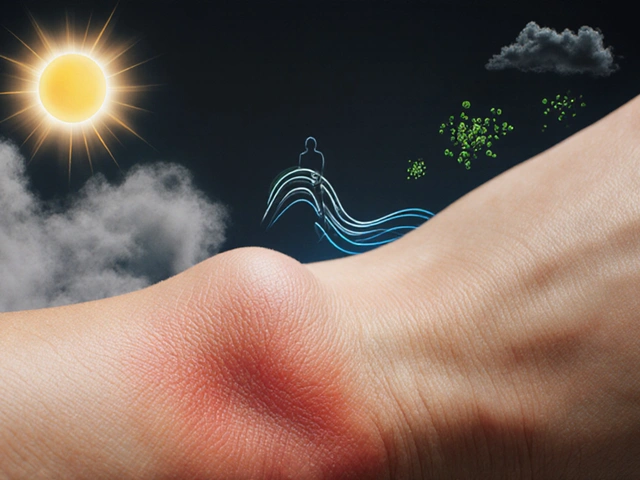
Environmental Skin Inflammation Trigger Identifier
Enter your details and click "Analyze Potential Triggers" to get personalized insights into environmental factors affecting your skin.
Common Environmental Triggers
UV Radiation
Sun exposure causes DNA damage and oxidative stress leading to inflammation.
Air Pollution
PM2.5 and pollutants penetrate skin causing oxidative damage and cytokine release.
Humidity
Extreme dry or wet conditions disrupt the skin barrier and microbiome.
Temperature Extremes
Heat or cold causes vasoconstriction and sweat-induced irritation.
Allergens
Pollen, dust mites, and pet dander activate immune responses.
Stress
Cortisol imbalance dysregulates immune function and increases sensitivity.
Ever wonder why a sudden flare‑up of eczema or acne seems to follow a hike in smog levels or a scorching summer? The answer lies in how the world around us talks to our skin. Below we break down the most common environmental culprits, explain the science behind the irritation, and give you a hands‑on plan to keep your skin calm.
Key Takeaways
- UV radiation, air pollution, humidity, temperature swings, allergens, stress, and microbiome disruption are the top environmental drivers of skin inflammation.
- Each factor triggers inflammation through different pathways - from oxidative stress to barrier breakdown.
- Protective habits (sun protection, indoor air filters, balanced humidity, stress management) cut flare‑ups by up to 40%.
- A simple daily checklist helps you spot and neutralise triggers before they flare.
- Tailoring skincare to your local climate and lifestyle yields the most lasting relief.
What Is Skin Inflammation?
When you see redness, swelling, itching, or a rash, your skin is reacting to a perceived threat. Skin Inflammation is a biological response that involves blood‑vessel dilation, immune‑cell activation, and the release of cytokines such as IL‑1β and TNF‑α. The process is meant to protect, but when it repeats or intensifies, conditions like eczema, psoriasis, and acne worsen.
Major Environmental Triggers
Not all irritants are created equal. Below are the seven most studied drivers, each with its own mechanism.
UV Radiation
Sunlight, especially UV‑B, damages DNA in skin cells, creating reactive oxygen species (ROS). The oxidative burst triggers the same inflammatory pathways that flare eczema. Even sub‑burn levels can suppress the skin barrier, making it leaky for allergens.
Air Pollution
Fine particulate matter (PM2.5) and nitrogen dioxide settle on the skin surface. They act like tiny “micro‑knives,” irritating the stratum corneum and prompting a cascade of cytokines. Studies from 2023‑2024 link high PM2.5 exposure to a 27% rise in eczema severity scores.
Humidity
Both excessively low and extremely high humidity disrupt the skin’s natural moisturizing factor (NMF). Dry air pulls water out of the epidermis, while humid conditions foster fungal overgrowth that can aggravate dermatitis.
Temperature Extremes
Sudden heat spikes cause sweat‑induced irritation, and cold snaps shrink blood vessels, reducing nutrient flow. The result is a compromised barrier that invites irritants.
Allergens
Pollen, dust‑mite proteins, and pet dander can infiltrate the skin, especially when the barrier is already weakened. The immune system treats them as invaders, releasing histamine and amplifying redness.
Stress
Psychological stress spikes cortisol, which paradoxically both suppresses and dysregulates immune responses. The net effect is an over‑reactive skin that reacts to even mild irritants.
Microbiome Disruption
Our skin hosts millions of friendly microbes that keep potential pathogens in check. Over‑use of harsh antiseptics or excessive sanitiser exposure wipes out these allies, allowing opportunistic bacteria to trigger inflammation.
How Each Factor Damages the Skin
Below is a side‑by‑side look at the biological routes each trigger uses.
| Trigger | Main Biological Pathway | Typical Skin Manifestations | Top Mitigation Strategy |
|---|---|---|---|
| UV Radiation | DNA damage → ROS → cytokine release | Redness, sunburn, barrier loss | Broad‑spectrum SPF 30+ daily |
| Air Pollution | Particulate penetration → oxidative stress | Persistent erythema, acne‑like bumps | Antioxidant‑rich cleanser + indoor air filter |
| Humidity (low/high) | Barrier dehydration or fungal overgrowth | Dry flakes or macerated rash | Humidifier (30‑50% RH) or breathable fabrics |
| Temperature Extremes | Vasoconstriction / sweat‑induced irritation | Cold‑induced chilblains or heat rash | Layered clothing, quick‑dry fabrics |
| Allergens | IgE‑mediated histamine release | Itchy patches, eczema flare | Allergen‑proof bedding, antihistamine creams |
| Stress | Cortisol imbalance → immune dysregulation | Worsening of existing conditions | Mind‑body practices, adequate sleep |
| Microbiome Disruption | Loss of commensal bacteria → opportunistic growth | Acne, contact dermatitis | Gentle, pre‑biotic cleansers |

Practical Mitigation Checklist
- Apply environmental factors skin inflammation‑focused sunscreen every morning, even on cloudy days.
- Use a HEPA air purifier in bedrooms; replace filters weekly during high‑pollution seasons.
- Maintain indoor humidity between 30% and 50% with a digital hygrometer.
- Dress in breathable, moisture‑wicking fabrics when temperatures swing.
- Swap heavy bedding for hypoallergenic covers; wash weekly in hot water.
- Practice 10 minutes of deep‑breathing or meditation each night to lower cortisol.
- Choose a gentle, pre‑biotic facial cleanser that supports the skin’s microbiome.
Skincare & Lifestyle Strategies Tailored to Your Environment
One‑size‑fits‑all products rarely work when the environment is the root cause. Below are targeted routines.
- Urban dwellers with high pollution: Start with an antioxidant serum (vitamin C, niacinamide) before moisturizer. Finish with a barrier‑repair cream containing ceramides.
- High‑altitude or sunny climates: Choose mineral‑based sunscreens (zinc oxide) that don’t irritate sensitive skin. Add a post‑sun soothing lotion with aloe and panthenol.
- Dry, desert‑like regions: Double‑moisturise - a hydrating serum (hyaluronic acid) followed by a rich emollient (shea butter or oat‑based cream).
- Humid tropical zones: Opt for lightweight, non‑comedogenic moisturisers. Keep hair away from the face to avoid sweat‑driven breakouts.
Remember, consistency beats occasional over‑the‑counter “miracle” fixes. Track your flare‑ups in a simple journal: note weather, stress level, diet, and skincare steps. Over a month you’ll see patterns and can fine‑tune your approach.
Frequently Asked Questions
Can indoor plants worsen skin inflammation?
Some plants release pollen or volatile organic compounds (VOCs) that can trigger allergies. If you notice flare‑ups after bringing a new plant home, try moving it to a well‑ventilated area or choose low‑allergen species like snake plant.
Is wearing masks for COVID‑19 protective for inflamed skin?
Masks can trap sweat and heat, creating a micro‑climate that aggravates acne or rosacea. Choose breathable fabrics (cotton) and change masks frequently. A light barrier cream under the mask can reduce friction.
How quickly can lifestyle changes reduce eczema flare‑ups?
Most people see a noticeable decline within 2‑4 weeks if they consistently follow the mitigation checklist and avoid primary triggers. Severe cases may need a dermatologist’s prescription to bridge the gap.
Do dietary changes affect skin inflammation caused by the environment?
Yes. Foods high in omega‑3 fatty acids (salmon, flaxseed) and antioxidants (berries, leafy greens) help counteract oxidative stress from UV and pollution. Reducing processed sugars also lowers systemic inflammation, which reflects on the skin.
Should I see a dermatologist if my skin reacts to the environment?
If over‑the‑counter measures and lifestyle tweaks don’t bring relief after a month, a dermatologist can prescribe targeted anti‑inflammatories, barrier‑repair ointments, or phototherapy tailored to your specific trigger profile.


Oh sure, the universe is just out to sabotage your skin – a little smog here, a dash of UV there, and boom, you’ve got a full‑blown rash 😜. Thanks, Mother Nature, for the endless inspiration for my skincare routine. Remember, the only thing worse than pollution is realizing you’ve been using the same cheap cleanser for years. Maybe try an antioxidant serum before you blame the weather. And if all else fails, just blame the planet and move to a desert island.
When we step back from the immediacy of a breakout and consider the broader tapestry of our environment, we begin to see that skin inflammation is not merely a reactionary flare but a dialogue between external stressors and our inner biochemistry. The philosophy of embodiment tells us that each molecule of ozone, each photon of ultraviolet light, and each microscopic pollen grain carries an intention that can tip the delicate equilibrium of our epidermal barrier. In this conversation, the skin serves both as a sentinel and a storyteller, narrating the cumulative history of exposure through redness, itching, and swelling. Modern research has illuminated how particulate matter, specifically PM2.5, can embed itself within the stratum corneum, initiating oxidative cascades that parallel the mechanisms of chronic inflammation seen in systemic diseases. Similarly, ultraviolet B radiation penetrates the superficial layers, provoking DNA photodamage that summons a cascade of cytokines, notably interleukin‑1β and tumor necrosis factor‑α, which act as messengers of distress. The thermodynamic fluctuations of temperature extremes are not benign either; they provoke vasoconstriction in the cold and hyperhidrosis in the heat, both of which can destabilize lipid bilayers and precipitate barrier dysfunction. Humidity, whether arid or oppressive, modulates the skin’s natural moisturizing factor, drying the surface in desert climates while fostering microbial overgrowth in tropical settings. Allergens such as pollen or dust mite proteins, when they breach a compromised barrier, engage IgE‑mediated pathways that unleash histamine, amplifying the itch‑scratch cycle. Psychological stress, often dismissed as merely “in the head,” actually raises systemic cortisol levels, which paradoxically can both suppress and dysregulate immune surveillance, leaving the skin vulnerable to otherwise minor irritants. The microbiome, a bustling metropolis of commensal organisms, can be displaced by over‑sanitization, allowing opportunistic pathogens to rise and incite inflammation. Each of these variables does not act in isolation; they intersect, creating synergistic effects that magnify the inflammatory response beyond the sum of their parts. Therefore, a truly holistic approach to managing skin inflammation must account for these intersecting axes, rather than focusing on a single culprit. By adopting a multi‑pronged strategy-incorporating antioxidant‑rich topicals, barrier‑repair lipids, and environmental controls such as air filtration-we can attenuate the cascade at several nodes simultaneously. Moreover, personal habit tracking, akin to a scientific journal, enables the identification of temporal patterns linking external conditions to flare‑ups, empowering individuals with actionable insight. In the grand scheme, recognizing skin inflammation as a nuanced conversation between body and environment transforms our approach from reactive band‑aid to proactive stewardship of the integumentary system.
From a dermatological perspective, the interplay between exogenous oxidants and the stratum corneum’s lipid matrix precipitates a dysregulated cytokine milieu, manifesting as acute erythema and chronic xerosis. When particulate matter (PM2.5) adheres to the epidermal surface, it serves as a vector for reactive oxygen species, which in turn activate NF‑κB signaling pathways. Concurrently, UV‑B photons induce pyrimidine dimers, triggering the nucleotide excision repair cascade that can be overwhelmed in high‑exposure scenarios. The resultant upregulation of IL‑6 and IL‑8 exacerbates vascular permeability, yielding the characteristic edema observed in dermatitis. Mitigating these processes necessitates a bifurcated regimen: topical antioxidants (e.g., vitamin C, niacinamide) to scavenge free radicals, and barrier enhancers (ceramides, cholesterol, fatty acids) to restore lamellar organization.
That overview really ties together the many pieces we often treat in isolation. It’s helpful to see how each factor can amplify the others over time.
Exactly, the synergy is where the real trouble lies. Keeping a simple log can unveil those hidden patterns.
Use a broad‑spectrum SPF every day. Follow with a ceramide‑rich moisturizer. Finish with an antioxidant serum.
But, consider, that, while SPF protects against UVB, it does not, by itself, mitigate the oxidative impact of PM2.5, which, as studies show, penetrates the skin barrier, leading to, chronic inflammation, especially in individuals with compromised barrier function, therefore, integrating antioxidant serums becomes, essential.
While sarcasm is entertaining, the underlying mechanisms are well‑documented and require evidence‑based interventions. Ignoring them won’t reduce the inflammatory load.
Your point underscores the need for clinical guidance when lifestyle tweaks fall short. Dermatologists can tailor therapies to individual trigger profiles.
Sure, but maybe the real problem is you’re over‑complicating simple skin care.