For every 10 prescriptions filled in the U.S., nine are for generic drugs. That’s not a coincidence-it’s the single biggest reason the American healthcare system hasn’t collapsed under the weight of rising drug prices. In 2024 alone, generic and biosimilar medications saved patients and the system $467 billion. Over the past decade, that adds up to more than $3.4 trillion in savings. That’s more than the entire annual GDP of Canada or Australia. And it’s happening quietly, behind the counter at your local pharmacy.
How Generics Cut Costs So Deeply
Generic drugs aren’t cheaper because they’re lower quality. They’re cheaper because they don’t need to recoup billions in research and marketing costs. Once a brand-name drug’s patent expires, other manufacturers can make the same medicine using the same active ingredients. The FDA requires them to prove they work the same way, in the same amount, in the same body. That’s it. No need for expensive clinical trials. No need to pay for TV ads telling you to ask your doctor about it. In 2024, Americans filled 3.9 billion generic prescriptions. That’s 90.2% of all prescriptions. But those generics made up just 12% of total drug spending. Meanwhile, brand-name drugs-only 10% of prescriptions-accounted for 88% of the money spent. That’s the math that makes generics so powerful. You’re getting the same medicine, but paying a fraction of the price. Take a common blood pressure pill like lisinopril. The brand version, Zestril, might cost $800 for a 30-day supply. The generic? Around $10. That’s a 98% drop. Multiply that by millions of patients, and you get billions in savings. In 2023, the top 10 most prescribed generics saved the system $89.5 billion. The 10 with the highest total savings? They saved $127 billion.Biosimilars: The Next Wave of Savings
Biosimilars are the next frontier. These are generic versions of biologic drugs-complex medicines made from living cells, like insulin, rheumatoid arthritis treatments, and cancer therapies. They’re harder to copy than simple pills, which is why they’ve taken longer to arrive. But they’re starting to make a huge difference. In 2024, biosimilars saved $20.2 billion. Since the first one hit the market in 2015, they’ve saved a total of $56.2 billion. That’s already more than the $54 billion projection experts made in 2021. And it’s accelerating. The biosimilar market grew 22.7% last year alone. Drugs like Humira and Enbrel, which used to cost over $70,000 a year, now have biosimilar alternatives priced at 30-50% less. That’s life-changing for people with chronic autoimmune diseases.Why the U.S. Saves More Than Other Countries
The U.S. has the highest rate of generic use in the developed world. Most European countries fill 60-80% of prescriptions with generics. The U.S.? 90.2%. Why? Because our system is built to push them. The 1984 Hatch-Waxman Act created the legal pathway for generics. It gave the first company to file for a generic version 180 days of exclusive rights-a reward for taking the risk. It also forced brand companies to list all their patents upfront, making it harder to hide behind endless legal tricks. That law didn’t just allow generics-it encouraged them. But it’s not perfect. Brand drugmakers have learned how to game the system. They file dozens of weak patents on minor changes-like a new coating or pill shape-to delay generics. This is called “patent thicketing.” A 2024 JAMA study found that just four drugs, protected by these tactics, cost the system over $3.5 billion in two years. Another trick? “Pay-for-delay.” Big pharma pays generic companies to hold off on launching their cheaper version. The Congressional Budget Office estimates this costs federal programs $3 billion a year.
Who’s Really Saving Money?
It’s not just patients. The biggest savings go to government programs. In 2024, generics saved Medicare $142 billion and Medicaid $62.1 billion. That’s money that didn’t have to come out of taxpayer pockets. Without generics, those programs would’ve been unaffordable. Private insurers saved too. Express Scripts, one of the biggest pharmacy benefit managers, reported $18.3 billion in savings in 2023 just from switching patients to generics. But here’s the catch: not all insurers push generics equally. Some Medicare Part D plans still steer patients toward brand-name drugs, even when generics are available. Why? Because PBMs get kickbacks from brand manufacturers. It’s a hidden incentive that hurts patients.What Patients Really Think
Most people who switch to generics are happy. A Drugs.com analysis of over 15,000 reviews found that 87% rated the cost as excellent or good. And 89% of patients who switched because of cost said they were satisfied with how the generic worked. But not everyone. Some report differences in side effects or effectiveness. That’s rare-but it happens. A small number of medications, especially those with narrow therapeutic windows (like seizure drugs or blood thinners), can behave slightly differently between brands. The FDA allows a 10-15% variation in absorption, which is usually harmless. But for some patients, even that small difference matters. That’s why doctors sometimes stick with brand names-for those rare cases. Reddit threads are full of stories. One person wrote about switching from a $800 brand to a $10 generic for their cholesterol drug. “I saved $9,000 a year,” they said. Another said their anxiety meds felt “off” on the generic. Their doctor switched them back. Neither scenario is the norm-but both are real.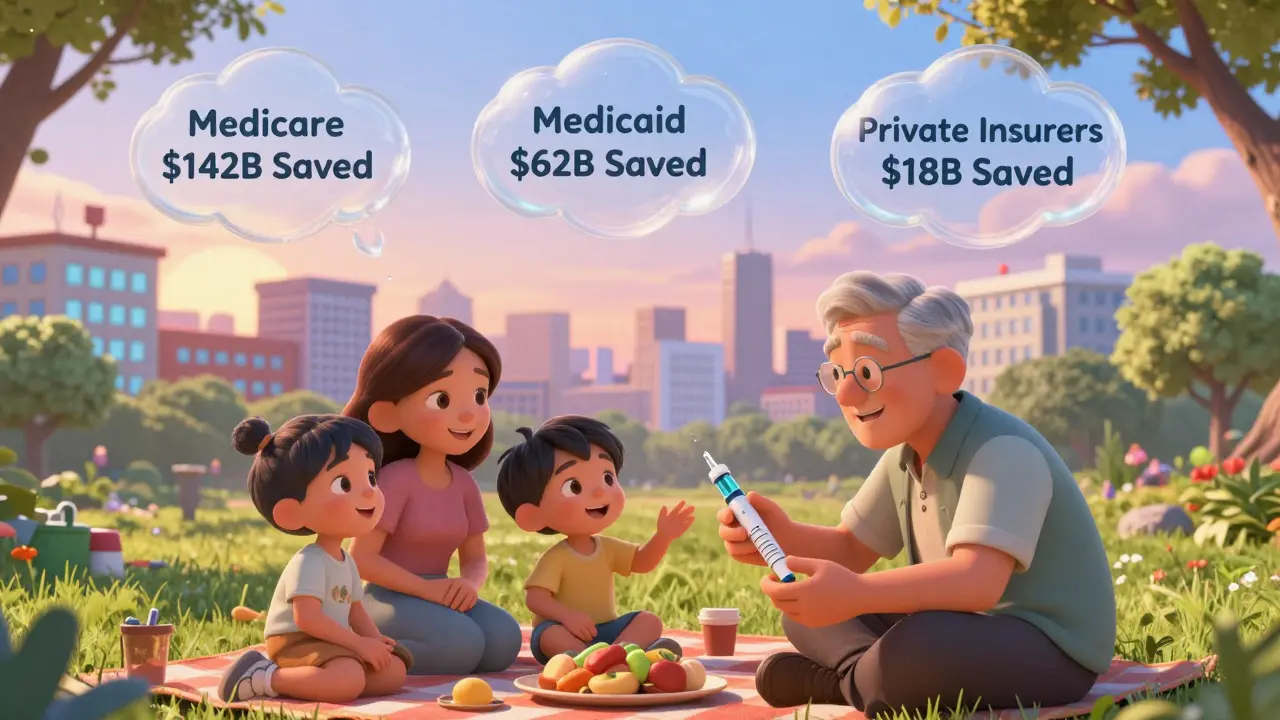


So let me get this straight - we’re celebrating a $3.4 trillion savings… while Big Pharma just invented a new pill shape and got 12 more years of monopoly? 🤡💊
Also, why does my generic lisinopril make me feel like a zombie but the brand version makes me feel like a superhero? Coincidence? I think not. 🌪️👁️🗨️
Oh wow, look at this feel-good fairy tale. The real story? The FDA lets generics in with 10-15% absorption variance - which is a joke for drugs like warfarin or levothyroxine. People die because they get switched without warning. And now you’re patting yourself on the back for saving $3.4 trillion while ignoring the human cost? You’re not a hero. You’re a statistician with a conscience deficit.
It is truly inspiring to witness the transformative impact of generic medications on public health infrastructure. The scientific rigor enforced by the FDA, coupled with the economic wisdom of the Hatch-Waxman Act, exemplifies how policy can align with humanitarian outcomes. One must acknowledge the diligence of manufacturers who produce life-sustaining drugs at minimal cost, and the pharmacists who ensure seamless substitution. This is not merely a financial triumph - it is a moral one. 🌍💙
Back home in Delhi, my aunt takes the same generic metformin - same batch, same manufacturer, just labeled differently. We pay $0.10 per pill there. Here? $5. Same science. Different capitalism. 🤷♂️🇮🇳🇺🇸
Also, why does everyone act like generics are some American invention? India makes 40% of the world’s generics. We’ve been doing this since the 70s. 😎
90.2% generic use? That’s not a win - it’s a failure of innovation. Every time you take a generic, you’re telling the pharmaceutical industry: ‘We don’t care about new drugs, just cheaper versions of old ones.’ You’re not saving healthcare - you’re killing its future. And biosimilars? They’re just knockoffs of expensive biologics made by companies who couldn’t afford to invent anything original. Congrats, you’ve optimized for mediocrity.
My insulin is $35 now because of biosimilars. No drama. No tears. Just life. 🙏
so like… the generic version of my anxiety med made me feel like i was drowning in slow motion? i switched back. my doc was like ‘lol’ and gave me the brand. i paid $800. worth it. also why do they even make generics if they dont work the same? 🤔
Interesting that you mention the 10-15% absorption variance without acknowledging the clinical implications for patients with epilepsy or heart failure. The FDA’s bioequivalence standard is statistically acceptable but clinically negligent for narrow-therapeutic-index drugs. Multiple studies (e.g., JAMA Internal Medicine, 2021) show increased hospitalization rates after forced generic switches in geriatric populations. This isn’t just about cost - it’s about risk stratification, and the system is ignoring it entirely.
While the statistical magnitude of savings presented in this article is undeniably impressive, it is imperative to interrogate the structural incentives that underpin this phenomenon. The concentration of generic manufacturing within ten corporations, the outsourcing of active pharmaceutical ingredient production to geopolitical risk zones, and the systemic failure to enforce post-market surveillance for bioequivalence deviations collectively constitute a precarious foundation for public health. The $3.4 trillion figure, while compelling, masks an increasingly brittle supply chain and a regulatory apparatus that prioritizes volume over vigilance. The absence of mandatory pharmacovigilance reporting for generic drugs - unlike brand-name counterparts - represents a dangerous asymmetry in risk accountability. Until these systemic vulnerabilities are addressed, the savings are not sustainable - they are merely deferred liabilities.