Imagine waking up with a constant ache in your shoulder, but no injury happened. You get an MRI, and it’s clean. Your doctor says it’s probably stress. Then the pain spreads to your head, your jaw, even down your arm. You’re told it might be a pinched nerve. But nothing helps. That’s not a mystery-it’s myofascial pain syndrome. And it’s hiding in plain sight, buried in tight bands of muscle you can’t see but can definitely feel.
What Exactly Are Trigger Points?
Trigger points aren’t just sore spots. They’re hyperirritable knots inside muscle tissue-small, firm nodules, about the size of a pea, that form when muscle fibers lock into a constant state of contraction. These aren’t random. They develop at the motor endplate, where nerves meet muscle. When that connection goes haywire, the muscle doesn’t relax. It stays clenched. And that’s when the pain starts.There are two kinds: active and latent. Active trigger points hurt on their own. You don’t even have to touch them-the pain is there, often radiating to other areas. Latent ones only hurt when you press on them. But even latent trigger points can limit your movement, make you stiff, or cause weakness without you realizing why.
Here’s what makes them tricky: they don’t hurt where they are. A trigger point in your upper trapezius (the muscle that runs from your neck to your shoulder) can make your temple throb. One in your jaw muscle can mimic a toothache. That’s why so many people get misdiagnosed-doctors look for nerve damage or joint problems, but the real source is tucked deep in a muscle.
Studies show trigger points are behind 85% of musculoskeletal pain visits in specialized clinics. The most common culprits? Upper trapezius, levator scapulae (neck muscle), and temporalis (jaw muscle). If you’re stuck at a desk, constantly hunched over, or clenching your jaw, you’re prime territory for these knots.
Why Trigger Points Hurt So Much
It’s not just about tightness. Inside a trigger point, the chemistry is off. Acetylcholine-normally used to tell muscles to contract-pours out at 10 to 100 times normal levels. Serotonin and noradrenaline spike. The pH drops to 4.3, making the area acidic. Blood flow gets squeezed shut. Oxygen starves the tissue. Waste products build up. And all of that? It turns the surrounding nerves into hyper-sensitive alarm systems.This creates a loop: pain → muscle spasm → more pain → more spasm. It’s self-sustaining. And it doesn’t go away with rest. Stretching alone won’t fix it. You need to break the cycle.
That’s why trigger points are often confused with fibromyalgia. But they’re not the same. Fibromyalgia tender points are symmetric, soft, and only hurt when pressed. Trigger points are in taut bands, cause referred pain, and can be isolated. One is a systemic issue. The other is a localized muscle malfunction.
How to Find Your Trigger Points
Finding them takes time and touch. You’re not looking for a single spot-you’re looking for a taut band. Run your fingers along your neck, shoulder, or upper back. If you feel a rope-like band with a hard nodule in the middle, that’s a likely trigger point.Press gently. If you feel pain that shoots elsewhere-like down your arm or into your ear-you’ve probably found it. The gold standard for confirmation is the local twitch response: when you press or snap the band, the muscle fibers jump involuntarily. That’s a clear sign you’ve hit the spot.
Common locations to check:
- Top of the shoulder (upper trapezius)
- Back of the neck, near the base of the skull (levator scapulae)
- Temples or jawline (temporalis)
- Inside the shoulder blade (rhomboids)
- Back of the thigh (hamstrings or gluteus medius)
Keep a pain journal. Note where you feel pain, when it started, and what makes it worse. Over time, patterns emerge. If your neck pain flares after driving, or your headaches follow long computer sessions, trigger points are likely involved.
Trigger Point Release Techniques That Actually Work
There’s no magic bullet, but several techniques have solid evidence backing them. The key? Consistency and pressure.Ischemic Compression
This is the simplest and most accessible. Use your fingers, a tennis ball, or a foam roller. Find the trigger point. Apply steady pressure until you feel a deep ache-not sharp pain. Hold for 30 to 90 seconds. You’ll feel the knot soften. Release slowly. Repeat 2-3 times per session. Do this daily.Studies show 60-75% of people get short-term relief. One patient on Reddit said, “Ischemic compression with a tennis ball helped my TMJ pain more than the $400 mouthguard.” That’s not an outlier. It’s science.
Dry Needling
This is when a thin needle is inserted directly into the trigger point. No medication. Just the needle. The goal? To get that local twitch response. When it happens, it resets the muscle’s electrical signal. Pain drops fast.Research shows 65-80% of patients get relief lasting 4-12 weeks. A Cochrane Review found dry needling works just as well as lidocaine injections-but without the cost or risk. It’s not for everyone. You need a trained professional. Look for a physical therapist or chiropractor certified in dry needling. Untrained providers can make things worse.
Spray and Stretch
Used mostly for neck and shoulder pain. A cooling spray (like ethyl chloride) is sprayed over the area of referred pain. Then, the muscle is gently stretched. The cold numbs the pain receptors, letting the muscle relax longer during the stretch. It’s effective for 50-65% of cervical cases.Instrument-Assisted Soft Tissue Mobilization (IASTM)
Tools like stainless steel or plastic scrapers are used to glide over the muscle. It breaks up adhesions and stimulates blood flow. Works well for chronic cases. Efficacy: 55-70%.Low-Level Laser Therapy (LLLT)
Uses specific wavelengths of light to reduce inflammation and promote healing at the cellular level. Not a quick fix. Requires multiple sessions. But for stubborn trigger points, it can reduce pain by 40-60% over time.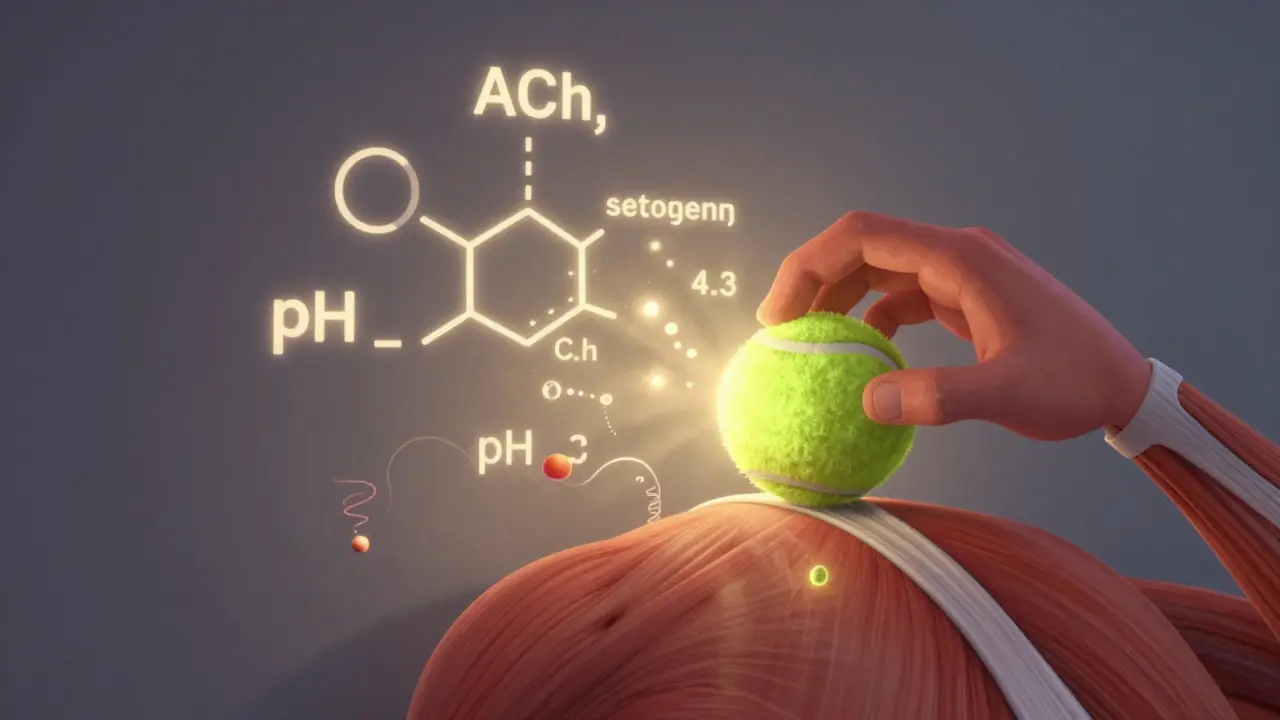
What Doesn’t Work (And Why)
Massage alone? Often not enough. If the therapist doesn’t target the trigger point specifically, you’re just rubbing the surface. Heat? Helpful before stretching, but won’t release the knot. Stretching cold muscles? Can make it worse.And here’s the big one: painkillers. NSAIDs don’t fix trigger points. They mask inflammation, but the muscle stays locked. Opioids? Completely ineffective. That’s why so many people get stuck in a cycle of prescriptions that don’t solve the real problem.
Home Care: Your Daily Routine for Lasting Relief
Treatment isn’t just about sessions. It’s about daily habits.- Self-compression: Use a tennis ball against a wall or floor. Target trigger points for 2 minutes per side, twice a day.
- Heat before stretching: Apply a warm towel or heating pad at 40-45°C for 15 minutes before stretching. This increases blood flow and makes muscles more responsive.
- Posture correction: If you work at a desk, set a timer. Every 30 minutes, roll your shoulders back, tuck your chin slightly, and take 3 deep breaths. Forward head posture increases trigger point risk by 3-5 times.
- Stretching: Focus on the muscles you’re targeting. For upper trapezius: tilt your head sideways, gently pull with your hand, hold 30 seconds. Repeat 3 times per side.
Compliance is the biggest predictor of success. In one study, 65% of patients who stuck with a daily home program saw 65% pain reduction in 12 weeks. Those who didn’t? Only 35% improvement.
When to See a Professional
You can manage mild cases on your own. But if:- Pain lasts more than 4 weeks despite self-care
- It’s radiating to your arm, leg, or head
- You’re having numbness, tingling, or weakness
- It’s interfering with sleep or daily tasks
-it’s time to get help. Look for a physical therapist, chiropractor, or pain specialist trained in myofascial release. Ask: “Do you use trigger point release techniques?” and “Can you show me the local twitch response?” If they don’t know what you’re talking about, find someone else.
Some providers offer certification. The American Academy of Physical Medicine and Rehabilitation has a 40-hour course with an 85% pass rate. That’s a good benchmark.
Why This Matters Now
The opioid crisis changed pain management. Doctors are looking for non-drug options. Trigger point therapy fits perfectly. It’s low-risk, low-cost, and works. In fact, referrals for manual therapies like this have grown 200% since 2015.And research is catching up. Scientists are now measuring chemicals in trigger points-substance P, bradykinin, TNF-alpha-all elevated in these knots. Ultrasound-guided release is being tested. Future treatments might combine dry needling with neuromodulation.
For now, the best tool you have is knowledge. Know your body. Know your triggers. And know that chronic muscle pain isn’t normal. It’s not just stress. It’s a treatable condition.
Frequently Asked Questions
Can trigger points cause headaches?
Yes. Trigger points in the temporalis (jaw muscle) or upper trapezius are common causes of tension headaches and migraines. The pain often feels like it’s coming from the scalp or behind the eyes, but the source is in the muscle. Releasing these points can reduce headache frequency by up to 70% in some patients.
Is dry needling the same as acupuncture?
No. Acupuncture is based on traditional Chinese medicine and targets energy meridians. Dry needling is grounded in anatomy and neurophysiology-it targets specific muscle trigger points. The needles are the same, but the technique, training, and intent are different. Dry needling requires specific certification in musculoskeletal therapy.
Can vitamin D deficiency cause trigger points?
Yes. Low vitamin D levels (below 20 ng/mL) are linked to a 60% higher risk of developing myofascial pain syndrome. Vitamin D helps regulate muscle function and inflammation. Correcting deficiency won’t erase trigger points, but it makes them easier to treat and less likely to return.
Why does my pain come back after treatment?
Trigger points return if the root cause isn’t addressed. Poor posture, repetitive movements, stress, or lack of stretching can reactivate them. About 40-60% of patients experience recurrence within 6 months without ongoing maintenance. Daily self-care is not optional-it’s essential.
Can I treat trigger points myself without tools?
Absolutely. Your fingers work just fine. Use your thumb or knuckles to press into tight bands. Hold for 60 seconds until you feel the knot release. It’s not about strength-it’s about sustained pressure. Many people get relief with just bodyweight pressure and consistent daily practice.
Are trigger points real, or just a myth?
While some researchers debate whether trigger points are distinct anatomical structures, the clinical evidence is undeniable. Millions of patients get relief from trigger point release. Studies confirm biochemical changes in these areas, and skilled practitioners consistently reproduce pain patterns. Whether you call them trigger points or muscle knots, the treatment works.
Next Steps
Start today. Pick one muscle group-maybe your shoulders or jaw. Spend 5 minutes finding the tight bands. Apply pressure. Stretch. Repeat daily. Track your pain on a scale of 1 to 10. In two weeks, you’ll know if this is working.If you’re still stuck, find a physical therapist who specializes in myofascial release. Don’t settle for generic massage. Ask for trigger point therapy. Your body’s telling you something. Listen to it.


I’ve been dealing with this for years-shoulder pain that shot down my arm like an electric shock. No injury, no herniated disc, just this relentless ache. I thought it was stress until I found a physical therapist who actually knew what a trigger point was. Turns out, my upper trapezius was basically a rock. I started using a lacrosse ball against the wall every morning before coffee. It’s not glamorous, but after six weeks? My headaches vanished. I didn’t even realize how much tension I was holding until it was gone. Now I do it twice a day, even if I’m just sitting at my desk. It’s not a cure, but it’s the closest thing I’ve found to reclaiming my body.
Also, vitamin D. I got tested and was borderline deficient. Took supplements for three months and noticed the knots were easier to release. Not magic, but it helps. Don’t ignore the basics.
And yes, I still roll out my jaw with a golf ball. Don’t judge me. I’m just glad I stopped blaming my neck on ‘bad posture’ and started treating the actual problem.
It’s wild how much we accept pain as normal. We wear tight shoes, hunch over screens, and then wonder why we feel like we’re made of concrete. This isn’t just ‘aging.’ It’s a signal. Listen to it.
I used to think massage was enough. It’s not. You have to target the knot. Not the area around it. The knot. That’s the difference between temporary relief and real change.
And if you’re thinking ‘I don’t have time’-you do. Five minutes a day. That’s it. I do mine while watching Netflix. No excuses.
Also, please stop telling people to ‘just stretch.’ Stretching a locked muscle without releasing the trigger point first? That’s like trying to un-knot a rope by pulling the ends. You’re just making it tighter.
Thank you for writing this. I wish I’d found it five years ago.
Now I tell everyone I know. Even my boss. He’s now using a tennis ball under his desk. Progress.
And yes, I still cry a little when I hit the right spot. It’s worth it.
Don’t give up. This stuff works. It’s just not sexy. And that’s why so many people miss it.
Wow, another one of these ‘trigger point’ miracle posts. You know what’s really causing your pain? Bad posture, bad lifestyle, and refusing to see a real doctor instead of playing with tennis balls in your garage. I’ve seen this exact thing a hundred times-people think they’re being ‘proactive’ by self-treating, but they’re just delaying real care. Dry needling? That’s not some folk remedy-it’s a medical procedure. Do you know how many people mess up their own muscles trying to ‘release’ things they don’t understand? You’re not a physical therapist. Stop pretending you are.
And vitamin D? Please. You think one supplement fixes everything? My cousin did that and ended up with kidney stones. Stop oversimplifying complex physiology. This isn’t a TikTok hack. It’s a chronic condition that needs professional diagnosis, not YouTube tutorials.
And don’t get me started on the ‘pain journal.’ That’s just a fancy way of saying ‘I’m obsessed with my discomfort.’
If you’re still in pain after all this, go see a rheumatologist. Not some ‘myofascial release specialist’ who got certified after a weekend seminar. Real medicine doesn’t come in a ball form.
While the phenomenological description of trigger points is compelling, the underlying pathophysiological mechanisms remain inadequately substantiated within the current biomedical paradigm. The assertion that acetylcholine concentrations are elevated by an order of magnitude lacks robust, peer-reviewed electrophysiological validation. Furthermore, the claim that pH drops to 4.3 in localized tissue is physiologically implausible given the body’s tightly regulated homeostatic buffering systems. The referenced Cochrane Review, while methodologically sound, does not establish causality, only correlation.
Additionally, the normalization of self-administered dry needling via household objects constitutes a significant public health concern. The absence of sterile technique, anatomical precision, and risk mitigation protocols invites iatrogenic complications, including pneumothorax, nerve damage, and hematoma formation. The proliferation of such practices under the guise of ‘empowerment’ is both ethically and epistemologically problematic.
One must also question the commercialization of this paradigm-many practitioners promote proprietary tools, apps, and courses with no regulatory oversight. The conflation of myofascial pain syndrome with fibromyalgia, while common in lay literature, is clinically inadvisable and risks diagnostic dilution.
While manual therapies may provide transient symptomatic relief, they do not constitute a curative or even disease-modifying intervention. A systems-based approach, integrating neurophysiological assessment and biomechanical re-education under licensed supervision, remains the gold standard. The reduction of chronic pain to ‘knots’ is not only reductive-it is dangerously misleading.
Thank you for sharing this. I’ve been in Nigeria for over 15 years working as a physiotherapist, and I can tell you-this is exactly what we see every day. People come in with neck pain, headaches, shoulder issues, and they’ve been told it’s ‘stress’ or ‘aging.’ But when we look closely, the trigger points are there-tight bands, referred pain, local twitch response. We don’t always have dry needling tools, but we use our hands, foam rollers, even broom handles. It works.
I’ve seen women who carry heavy buckets on their heads develop trigger points in their levator scapulae. Men who sit all day on motorbikes get them in their glutes. It’s universal. The body doesn’t care if you’re in Lagos or LA-it reacts the same way to tension.
And you’re right about vitamin D. In our climate, many people don’t get enough sun. We test everyone now. If their level is below 30, we treat it. It helps.
But the biggest thing? Consistency. One man told me he did the tennis ball thing every night before bed. After three months, he stopped taking painkillers. He said, ‘I didn’t know I was holding my shoulders like I was afraid of the sky.’
It’s not magic. It’s just human. And we’re all just trying to move without pain.
Thank you for saying this so clearly. More people need to hear it.
Bro this is spot on. I’ve been sitting at my laptop for 12 hours a day since 2020. My neck felt like concrete. Tried massage, acupuncture, even a chiropractor who just cracked my back and charged me $120. None of it helped.
Then I found a YouTube video about trigger points. Used a lacrosse ball on my shoulder for 3 minutes. Felt like a knife going in. But then… it released. Like a sigh. My head stopped feeling heavy.
Now I do it every morning. No tools. Just my thumb. Press. Hold. Breathe. Repeat.
Also, stop drinking soda. Seriously. Sugar = inflammation = more knots. I cut it out. My jaw stopped clicking. Weird, right?
And yeah, I know it’s not ‘scientific’ enough for some people. But it works. And I’m not dying. So I’m gonna keep doing it.
I found mine in my jaw. I didn’t even know I was clenching. Thought it was a tooth. Went to the dentist. He said nothing’s wrong. Then I read this. Tried pressing under my cheekbone. Felt like a marble. Pressed for a minute. Felt my whole face go warm. Then my headache just… left.
I’ve been doing it every night. I don’t even think about it anymore. It’s just part of brushing my teeth now.
Also, stop sleeping on your stomach. Just stop.
It's interesting how the body holds memory in muscle tissue. I think trigger points are less about biochemistry and more about emotional residue. We hold grief, stress, fear in our shoulders, our jaw, our hips. The knots aren't just physiological-they're psychological. When we release them, we're not just relaxing muscle fibers-we're letting go of something we've been carrying silently for years.
I used to think it was all about posture. But after my mom passed, my upper back locked up like a vault. No amount of stretching helped. It wasn't until I started pressing into the knots while crying that they began to soften. It wasn't the pressure. It was the permission to feel.
Maybe that's why it works. Not because of acetylcholine. But because we finally stop pretending we're okay.
Just a thought. I'm not a doctor. But I've lived this.
Okay but have you considered that trigger points are just a distraction tactic by Big Pharma to keep you from realizing that 5G towers are causing chronic muscle tension? They don’t want you to know that EMF radiation creates micro-spasms in your fascia. The same companies that sell you NSAIDs also sell the ‘dry needling’ devices. It’s all connected.
And vitamin D? That’s a red herring. The real fix is grounding-walking barefoot on concrete. The earth’s negative ions neutralize the positive charge buildup from your devices. That’s why the pain goes away after you walk outside. The science is suppressed because it can’t be patented.
Also, the ‘local twitch response’? That’s just your muscle reacting to the fear of being poked. Your nervous system is tricking you into thinking it’s working. It’s placebo with a needle.
My cousin’s neighbor’s dog had the same symptoms. They cured it by placing a crystal under its bed. I’m not joking. You want real relief? Ditch the tennis balls. Get a shungite. It absorbs EMF. I swear on my life.
And don’t tell me you’ve ‘tried everything.’ You haven’t tried the truth.
The biochemical cascade described here is oversimplified and misleading. Elevated substance P and TNF-alpha are systemic markers of chronic inflammation, not localized trigger point phenomena. The notion that a single muscle knot can produce such a distinct neurochemical signature ignores the broader neuroimmune axis. The data cited lacks control for confounding variables-stress, sleep, cortisol levels, gut permeability-all of which modulate pain perception.
Moreover, the emphasis on ‘self-treatment’ normalizes the medicalization of everyday discomfort, shifting responsibility away from structural societal issues-sedentary work environments, wage labor, poor ergonomics-onto the individual’s ability to ‘press harder’ with a ball.
It’s not that the techniques don’t provide temporary relief. They do. But they’re palliative, not curative. And by framing this as a personal solution, we ignore the systemic failure to provide accessible, preventative healthcare.
This isn’t about knots. It’s about a culture that rewards productivity over well-being-and then sells you a foam roller to cope with the consequences.
Okay, so you’ve got a knot. Big deal. Now what? You gonna sit there and press on it for the rest of your life? Nah. You need a plan. Here’s what I did:
Day 1: Found the trigger point with a tennis ball. Felt like death.
Day 2: Did it again. Still hurt. But less.
Day 3: Added heat before. Woke up feeling like a human.
Day 7: Started doing shoulder rolls every hour. Set a timer on my phone. Even at work.
Day 14: My neck didn’t crack when I turned my head. That was the moment I knew.
Now I do it every morning. No excuses. I’m not ‘healing.’ I’m maintaining. This isn’t a cure-it’s a lifestyle.
And guess what? I stopped taking ibuprofen. Not because I’m brave. Because I didn’t need it anymore.
You don’t need a degree. You don’t need a $200 device. You just need to show up. Every day. Even if it’s just for 90 seconds.
So stop reading. Go find your knot. Press. Hold. Breathe.
Then come back here in two weeks and tell me you’re still in pain.
I’ll be waiting.
Chris, you’re right. I did it. Two weeks in. Pain went from 8/10 to 2/10. I didn’t even realize how much I was holding my breath until I stopped. I’m not ‘cured.’ But I’m not miserable anymore.
Also, I started walking 10 minutes a day. No phone. Just me and the sidewalk. It helped more than I expected.
Thanks for not just telling me to ‘try harder.’ You showed me how.