Clopidogrel-PPI Interaction Calculator
Select Your PPI
Interaction Result
Select a PPI to see the interaction impact
If you’re taking clopidogrel to prevent heart attacks or strokes, and your doctor also prescribed omeprazole for heartburn, you might be unaware of a hidden conflict between these two common drugs. It’s not a simple side effect-it’s a pharmacological clash happening inside your liver, where your body tries to activate clopidogrel but omeprazole gets in the way. This isn’t theory. It’s backed by decades of research, FDA warnings, and real-world outcomes that have changed how doctors prescribe these medications.
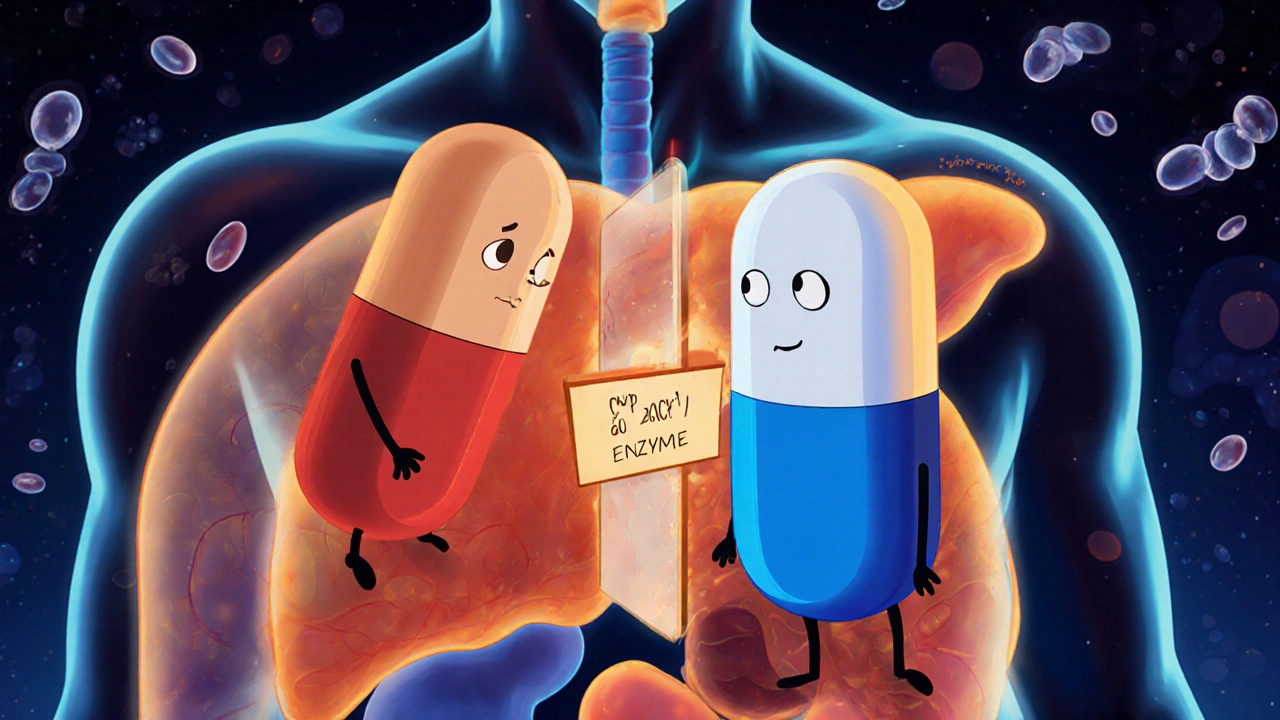
How Clopidogrel Actually Works
Clopidogrel doesn’t work right after you swallow it. It’s a prodrug, meaning it’s inactive until your liver turns it into something that blocks platelets from clumping together. That transformation relies almost entirely on one enzyme: CYP2C19. Without it, clopidogrel sits there, useless. About 30% of people-especially those of East Asian descent-have genetic variants that make this enzyme less effective. But even if your genes are normal, another drug can shut down CYP2C19: omeprazole.
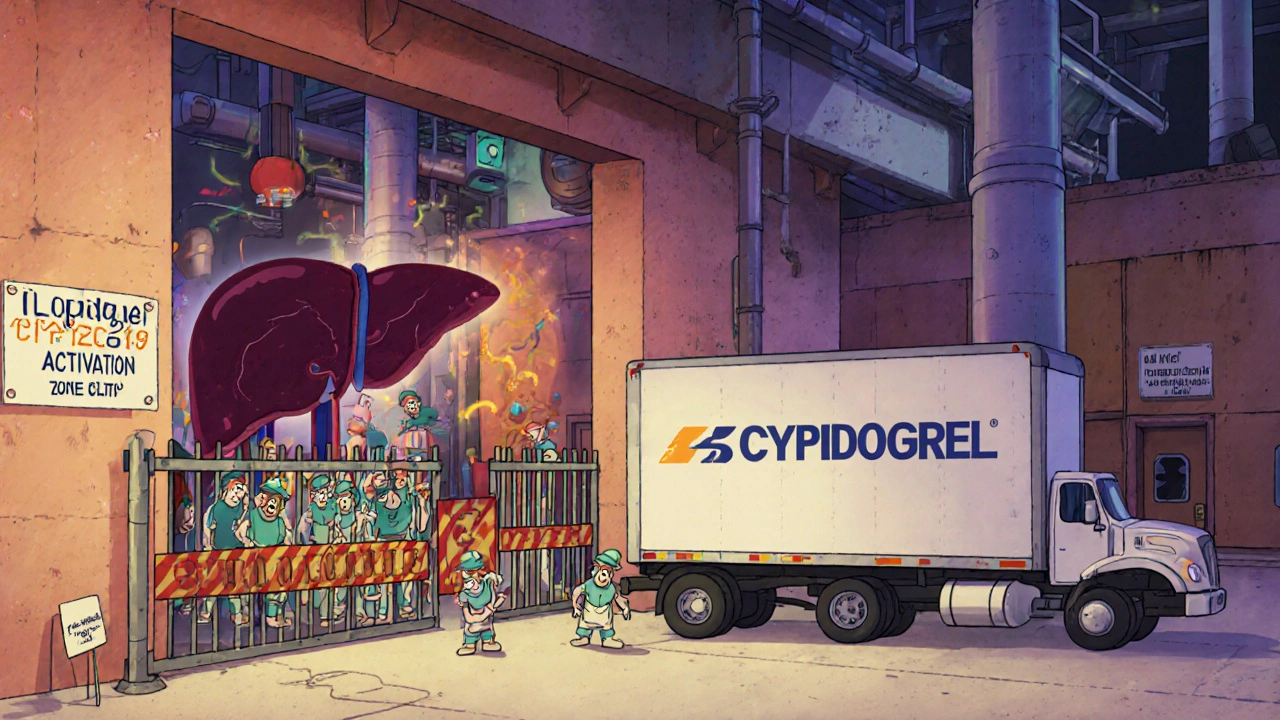
Why Omeprazole Is the Problem
Omeprazole is a proton pump inhibitor (PPI), designed to reduce stomach acid. But it doesn’t just sit in your stomach. It gets absorbed into your bloodstream and ends up in your liver, where it binds tightly to CYP2C19. It’s like parking a truck in front of a factory entrance-no other vehicles (like clopidogrel) can get in. Studies show that a standard 20mg daily dose of omeprazole cuts the amount of active clopidogrel metabolite in your blood by 32%. At 80mg, that jump to 49%. That’s not a small drop. That’s enough to reduce how well clopidogrel stops clots.
The FDA issued a safety alert in 2009 after multiple studies confirmed this. One key paper by Sibbing et al. in 2008 showed that patients taking both drugs had significantly higher rates of stent thrombosis-a dangerous clot inside a heart stent. The message was clear: omeprazole and clopidogrel don’t play well together.
Not All PPIs Are Created Equal
Here’s where things get practical. Not every acid reducer is the same when it comes to CYP2C19. Omeprazole and its close relative, esomeprazole, are the worst offenders. Lansoprazole is a bit better. Pantoprazole? Much weaker. Rabeprazole? Even less interference. And ilaprazole, a newer PPI not yet widely available in the U.S., shows almost no effect at all.
Here’s a quick comparison based on clinical data:
| PPI | Daily Dose | Reduction in Clopidogrel Active Metabolite | Clinical Risk Level |
|---|---|---|---|
| Omeprazole | 20 mg | 32% | High |
| Omeprazole | 80 mg | 49% | Very High |
| Esomeprazole | 40 mg | 40% | High |
| Lansoprazole | 30 mg | 5% | Low |
| Pantoprazole | 40 mg | 14% | Very Low |
| Rabeprazole | 20 mg | 28% | Moderate |
| Ilaprazole | 10 mg | Minimal | Lowest |
So if you need a PPI while on clopidogrel, pantoprazole is your safest bet. Rabeprazole is acceptable if pantoprazole isn’t available. Omeprazole and esomeprazole? Avoid them.
Does This Actually Lead to More Heart Attacks?
This is where the debate gets messy. Some large studies say yes. A 2014 meta-analysis of over 270,000 patients found that combining clopidogrel with any PPI increased the risk of heart attack or stroke by 27%. Omeprazole alone pushed that risk up 33%. But then came the COGENT trial-a randomized study of 3,761 people-that found no difference in heart events between those taking omeprazole and those who didn’t. The FAST-MI Registry, tracking over 2,700 patients, also found no increased risk.
Why the contradiction? One big reason: genetics. The negative effects are strongest in people with CYP2C19 loss-of-function alleles. These variants are common in Asian populations (up to 35%) and less so in Caucasians (20-25%). A Korean study showed omeprazole reduced clopidogrel’s effect by 54% in intermediate metabolizers-people who already have reduced enzyme activity. For them, the interaction isn’t just theoretical-it’s dangerous.
Meanwhile, people with normal CYP2C19 function may not see much impact. That’s why some doctors argue the risk is overstated. But here’s the thing: you don’t know your genotype unless you get tested. And if you’re on clopidogrel after a stent or heart attack, you can’t afford to guess.
What Should You Do?
Don’t stop your meds. Don’t switch on your own. But do ask your doctor these questions:
- Is omeprazole the only option for my stomach issues?
- Have I been tested for CYP2C19 variants?
- Could I switch to pantoprazole instead?
- Is there a non-PPI alternative, like famotidine (an H2 blocker)?
The American College of Gastroenterology and the Clinical Pharmacogenetics Implementation Consortium both recommend pantoprazole as the preferred PPI when clopidogrel is needed. If you’re a poor or intermediate metabolizer, they suggest switching from clopidogrel to prasugrel or ticagrelor-two newer antiplatelet drugs that don’t rely on CYP2C19.
And timing doesn’t help. Some people think taking clopidogrel in the morning and omeprazole at night will avoid the interaction. It won’t. The enzyme inhibition lasts all day. It’s not about when you take them-it’s about whether they’re both in your system.
What’s Changing in 2025?
Prescribing habits have shifted since the FDA warning. In the U.S., omeprazole prescriptions with clopidogrel dropped by 65% after 2009. Pantoprazole use rose by 42%. More cardiology clinics are now doing CYP2C19 genetic testing-74% according to the ACC’s 2023 data. That’s not routine everywhere, but it’s growing.
Drug development is catching up, too. Three new antiplatelet agents are in Phase II trials as of late 2024, designed specifically to avoid CYP2C19 metabolism. And ilaprazole, the PPI with the weakest inhibition, is gaining attention in Asia and may soon be available elsewhere.
The bottom line? The interaction is real. The risk isn’t the same for everyone. But if you’re on clopidogrel and need acid control, don’t default to omeprazole. Ask for alternatives. Push for testing if you’re high-risk. Your heart might depend on it.
Can I take omeprazole and clopidogrel together if I take them at different times of day?
No. Separating the doses-like taking clopidogrel in the morning and omeprazole at night-doesn’t prevent the interaction. Both drugs are metabolized by the same liver enzyme, CYP2C19, and omeprazole’s inhibition lasts all day. The effect is not about timing; it’s about the presence of omeprazole in your system blocking the enzyme needed to activate clopidogrel.
Is pantoprazole really safer than omeprazole with clopidogrel?
Yes. Multiple studies show pantoprazole has minimal impact on clopidogrel’s activation. At a 40mg daily dose, it reduces the active metabolite by only about 14%, which is not considered clinically significant. Major guidelines from the American College of Gastroenterology and the European Society of Cardiology recommend pantoprazole as the preferred PPI for patients on clopidogrel.
What if I need a PPI but I have a CYP2C19 gene variant?
If you’re an intermediate or poor metabolizer of CYP2C19, clopidogrel may not work well even without omeprazole. Adding omeprazole makes it worse. The best option is to switch to an alternative antiplatelet like prasugrel or ticagrelor, which don’t rely on CYP2C19. Then you can safely use any PPI, including omeprazole, if needed for stomach protection.
Are there non-PPI options for stomach protection while on clopidogrel?
Yes. H2-receptor antagonists like famotidine (Pepcid) or ranitidine (though ranitidine is no longer available in many places) are effective for reducing stomach acid and don’t interfere with CYP2C19. They’re often recommended as alternatives when PPIs are risky. For mild symptoms, antacids like calcium carbonate can also be used occasionally without interaction concerns.
Why do some studies say PPIs don’t increase heart attack risk?
Some large observational studies, like the FAST-MI Registry and COGENT trial, found no increased risk of heart events. But these studies didn’t always account for genetic differences. The risk is strongest in people with CYP2C19 loss-of-function alleles-about 30% of the population. If those patients are mixed in with people who metabolize clopidogrel normally, the overall effect looks small. That’s why personalized medicine and genetic testing are becoming more important.

Wow, this is such an important post-seriously, why isn’t this taught in med school? I’m from India, and I’ve seen so many patients on clopidogrel get prescribed omeprazole like it’s candy! And then they come back with stent issues… It’s not just about the drug-it’s about awareness! The data here is crystal clear, and honestly, if your doctor doesn’t know this, you should find a new one. Pantoprazole is the way to go, no debate. Also, CYP2C19 testing? Should be routine for anyone with cardiac history. Period.
Let’s be real-this post is technically accurate, but it’s also dangerously oversimplified. You’re implying that all PPIs are interchangeable, but the clinical data is messy. The COGENT trial showed no increase in MACE events. The FDA warning? Based on observational studies with confounding variables. And let’s not forget: many of these patients are on aspirin too, which itself inhibits platelets. The real issue? Overinterpretation of pharmacokinetic data as clinical outcome. Don’t throw out omeprazole without evidence of harm in your specific population.
Actually, I’ve been researching this for my dad-he had a stent last year and is on clopidogrel. He was on omeprazole for years. I dug into the FDA alert and found the Sibbing paper. Then I checked the 2023 ACC guidelines. Turns out, pantoprazole is recommended, but only if you’re a poor metabolizer. My dad’s genetic test came back normal. So maybe we don’t need to panic? I’m not saying ignore it-but don’t switch meds based on fear. Talk to your cardiologist. Maybe get tested. Don’t just trust Reddit.
Thank you for this 🙏 I’ve been on clopidogrel since my bypass in 2020 and was on omeprazole until last month. My pharmacist flagged it-she’s a wizard. Switched to pantoprazole and my heartburn’s still gone. No more ‘acid reflux panic’ 😅 Also, I got tested for CYP2C19-normal metabolizer. But I’m keeping pantoprazole anyway. Better safe than sorry. And hey, famotidine works too if you want to go old-school. Just say no to omeprazole with clopidogrel. 🚫💊
Hi everyone-I’m a nurse in Chicago and I see this every single day. Patients get so scared when you tell them to stop omeprazole. They think they’ll die from heartburn. But guess what? Most of them don’t even need a PPI. H2 blockers like famotidine work great, and they’re way cheaper. And if they do need something stronger? Pantoprazole. Always. I’ve had patients cry because they loved omeprazole. I get it. But your heart matters more than convenience. Please, if you’re on clopidogrel-ask for alternatives. You’ve got options. You’re not alone.
This is why America’s healthcare is falling apart. Some Indian guy wrote a blog and now everyone’s flipping out over a drug interaction? We’ve got real problems-border security, inflation, crime-and we’re worrying about whether omeprazole blocks a liver enzyme? Get a grip. If you’re on clopidogrel, you’re already high-risk. Stop blaming the PPI. Take your meds. Stop reading Reddit. And for God’s sake, don’t let some PhD from Stanford tell you what to do. Your doctor knows your body-not some algorithm.
The pharmacokinetic data presented is methodologically sound and aligns with current consensus in clinical pharmacology literature. However, the clinical translation remains contentious due to heterogeneity in study populations, particularly regarding CYP2C19 genotyping status. The absence of genotype stratification in meta-analyses such as the 2014 study likely attenuates effect size estimates. Further prospective, genotype-stratified RCTs are warranted before definitive clinical recommendations can be universally applied.
Listen up, folks-this isn’t just some nerdy drug talk. This is LIFE OR DEATH. I’ve seen two friends lose stents because their doctors didn’t know this. One guy was on omeprazole like it was a vitamin. He didn’t even know what CYP2C19 meant. Now he’s got a second stent, a scar on his chest, and a PTSD diagnosis. Don’t be that guy. Switch to pantoprazole. Get tested. Ask your doc if they’ve even heard of the ACC guidelines. If they haven’t, go somewhere else. Your heart didn’t come with a warranty. Protect it like your life depends on it-because it does.
This is an excellent, well-referenced summary. I’ve worked in cardiology for 18 years and I’ve seen this play out too many times. The key point often missed is that the interaction is not binary-it’s a spectrum. For a 72-year-old with stable CAD and no prior events, the risk may be negligible. For a 55-year-old with a drug-eluting stent and diabetes? Absolutely avoid omeprazole. And yes, timing doesn’t matter. The enzyme is inhibited for 24 hours. I always tell patients: ‘If you’re taking something for your heart, treat it like a sacred trust. Don’t gamble with it.’
Oh my GOD, I knew this was happening! I told my cousin’s husband, ‘DON’T TAKE OMEPRAZOLE WITH CLOPIDOGREL!’ He laughed at me-he’s a ‘doctor’ in Bangalore, thinks he knows everything! Two months later, he had a stent thrombosis. Now he’s on ticagrelor, and his wife is crying every night. I’m not a doctor, but I read the internet, and I saved his life! Why do people ignore warnings? Why? Because they think they’re too smart? I’m just saying… I told you so. 🙃
I just switched from omeprazole to pantoprazole last week after reading this. My heart feels lighter… not just literally 😅 I was so scared I’d have to live with heartburn forever. Turns out, pantoprazole works just as well. And now I feel like I’m doing something right for my body. You guys are the real MVPs for sharing this info. Keep posting stuff like this-it saves lives. Love you all!
While the pharmacological mechanism is indeed well-documented, the clinical relevance of this interaction remains empirically unsubstantiated in large-scale, prospective, randomized controlled trials with adequate power. The reliance on observational data and pharmacokinetic surrogates is methodologically insufficient to justify a paradigm shift in prescribing practices. One must question whether this constitutes evidence-based medicine-or merely pharmacological dogma masquerading as consensus.
So… pantoprazole = good, omeprazole = bad. Got it. 😎 I’ve been on both and didn’t notice a difference, but hey, if the science says switch, I’ll switch. I’m not risking a heart attack over a $5 pill. Also, famotidine is basically the OG heartburn fix. Still works. Still cheap. Still doesn’t mess with your liver. So yeah… I’m down with this. 👍
Why are we even talking about this? In India, everyone takes omeprazole with clopidogrel. No one dies. My uncle took both for 7 years and still runs marathons. This is just Western over-medicalization. You think your liver is so special? We don’t need genetic tests. We don’t need fancy PPIs. Just take your pills. Stop reading blogs. Stop being scared. Your body knows what to do. Omeprazole is cheap. Pantoprazole? Expensive. Why waste money? This post is fear-mongering disguised as science.