G6PD Safety Calculator for Primaquine
Primaquine Safety Calculator
Enter your G6PD enzyme activity percentage to determine if Primaquine treatment is safe.
How It Works
Based on WHO guidelines:
- Safe ≥ 30% - Primaquine can be used with standard dosing
- Caution Required 20-30% - Reduced dosing or alternative may be needed
- Unsafe ≤ 20% - Primaquine should not be used
Alternative Options
If G6PD is low:
Results Will Appear Here
Enter your G6PD percentage and click "Check Safety" to see the results.
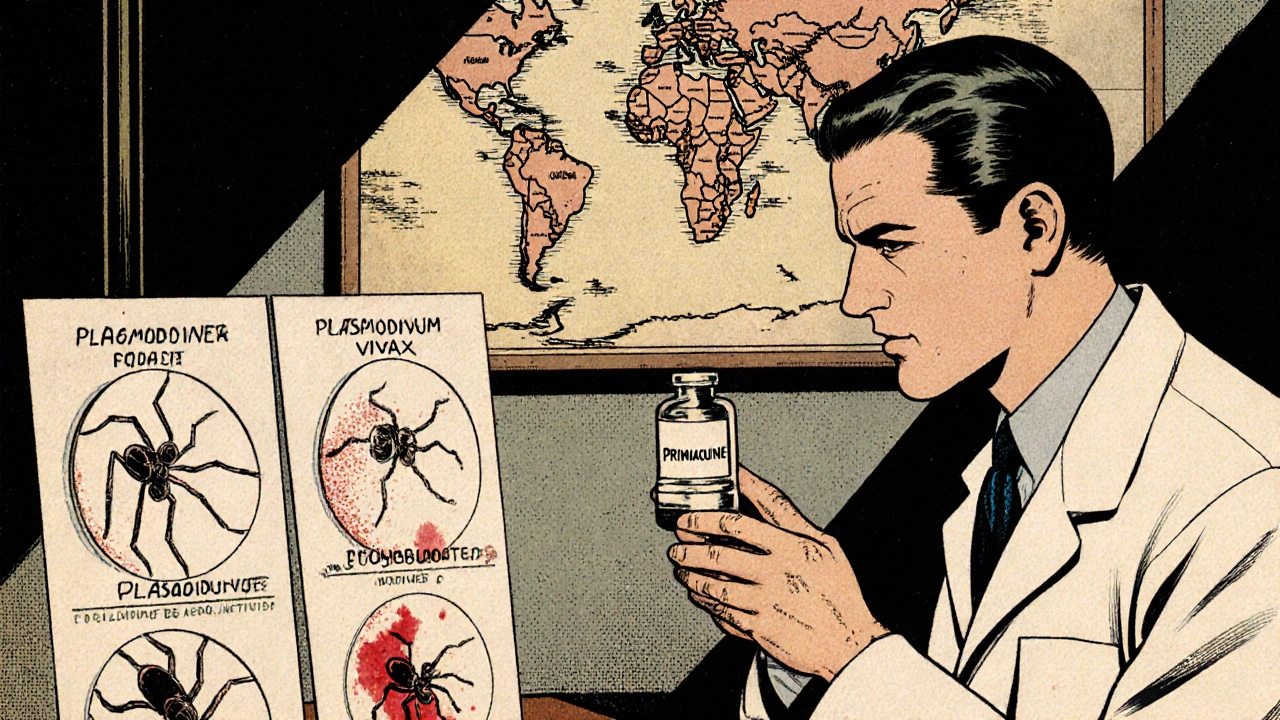
When you hear the name Primaquine, malaria is probably the first disease that comes to mind. That’s because the drug has been a frontline tool against Plasmodium vivax and Plasmodium ovale for decades. But researchers are now looking at how the same chemistry can be leveraged to curb other mosquito‑borne threats - from dengue to Zika - and what that means for public‑health strategy worldwide.
What is Primaquine?
Primaquine is an 8‑aminoquinoline antimalarial discovered in the 1940s. Its primary strength lies in targeting dormant liver stages, called hypnozoites, that cause relapses weeks or months after the initial infection. In the UK, the drug is listed under the National Institute for Health and Care Excellence (NICE) guidelines for radical cure of P. vivax malaria.
How Primaquine Stops Relapse
Once a mosquito injects sporozoites into a person, they travel to the liver. For P. vivax and P. ovale, a fraction of these parasites become hypnozoites - essentially sleeping cysts that can reactivate. Primaquine interferes with the parasite’s mitochondrial electron transport chain, wiping out these hidden forms and preventing future blood‑stage infections.
Beyond Malaria: Targeting Other Mosquito‑Borne Illnesses
While Primaquine was never intended for viruses, its broad‑spectrum activity against certain protozoa has sparked interest in related diseases transmitted by Aedes mosquitoes. Here’s where the research gets exciting:
- Dengue: Laboratory studies show Primaquine can reduce the replication of dengue virus in liver cells, limiting the severity of secondary infections.
- Zika: Early‑phase trials suggest a modest drop in viral load when Primaquine is added to standard supportive care, potentially decreasing the risk of congenital transmission.
- Chikungunya: In mouse models, the drug lowered inflammation markers, hinting at a role in managing the painful joint symptoms that can linger for months.
- Yellow fever: Though not a direct antiviral, Primaquine’s ability to clear parasitic co‑infections (e.g., filarial worms) may improve overall immune response during outbreaks.
These findings are still preliminary, but they point to a future where a single pill could help curb multiple diseases that share the same vector.
Safety First: The G6PD Connection
The biggest obstacle to widescale Primaquine use is its hemolytic risk in people with glucose‑6‑phosphate dehydrogenase (G6PD) deficiency. This genetic condition, affecting roughly 400million people globally, impairs red‑blood‑cell resilience. When exposed to Primaquine, affected individuals can experience rapid hemolysis, leading to anemia and, in severe cases, kidney failure.
Guidelines from the World Health Organization (WHO) now recommend point‑of‑care G6PD testing before any primaquine‑based regimen. Point‑of‑care devices cost underUS$5 and deliver results in 10minutes, making it feasible for field teams in endemic regions.
Resistance and the Next Generation
Resistance to antimalarials has historically undermined control programs. So far, Primaquine remains effective against hypnozoites, but mutations in the pfcrt and pvmdr1 genes have been observed, raising concerns for future loss of efficacy.
A newer 8‑aminoquinoline, Tafenoquine, offers a single‑dose alternative. However, its safety profile in G6PD‑deficient patients mirrors Primaquine’s, and it costs roughly ten times more. The table below highlights key differences.
| Attribute | Primaquine | Tafenoquine |
|---|---|---|
| Dosage regimen | 14‑day course (0.25mg/kg daily) | Single dose (300mg) |
| Cost (per treatment) | ≈US$2-3 | ≈US$25-30 |
| G6PD safety threshold | ≥30% activity | ≥70% activity |
| Efficacy against hypnozoites | >95% radical cure | ~90% radical cure |
| Availability in endemic countries | Widely stocked | Limited, pending regulatory approval |
Practical Guidance for Clinicians
- Screen every patient for G6PD deficiency using a rapid test. If activity is <30%, consider alternative strategies or a supervised low‑dose regimen.
- Prescribe the standard 14‑day Primaquine course for confirmed P. vivax infection, adjusting for weight and renal function.
- If treating a suspected co‑infection (e.g., dengue) in a malaria‑endemic area, discuss the experimental nature of Primaquine’s antiviral benefits with the patient and obtain informed consent.
- Monitor hemoglobin levels on day7 and day14 to catch early signs of hemolysis, especially in populations with high G6PD variant prevalence.
- Document adverse events and report them to local pharmacovigilance centers; this data fuels WHO’s safety database.
Key Takeaways
- Primaquine remains the gold standard for clearing malaria hypnozoites.
- Emerging lab data suggest it may also blunt the severity of dengue, Zika, and chikungunya, though large‑scale trials are pending.
- G6PD testing is non‑negotiable; without it, the drug’s benefits are outweighed by hemolytic risk.
- Resistance is not yet a major issue, but surveillance should continue alongside newer agents like tafenoquine.
- Integrating Primaquine into multi‑disease vector control programs could simplify logistics in resource‑limited settings.
Frequently Asked Questions
Can Primaquine prevent dengue infection?
Current evidence shows Primaquine may reduce viral replication in laboratory models, but it is not approved as a dengue prophylactic. Clinical trials are ongoing to assess whether adding a short course to standard supportive care improves outcomes.
What is the safest dosage for G6PD‑deficient patients?
For patients with 30‑70% G6PD activity, a supervised low‑dose regimen (0.125mg/kg daily for 14days) can be considered, but it must be accompanied by close hematologic monitoring.
How does Primaquine compare to Tafenoquine in terms of cost?
Primaquine costs a few dollars per treatment, making it affordable for most low‑income health programs. Tafenoquine, by contrast, is priced at roughly ten times higher, limiting its accessibility in many endemic regions.
Is there any risk of resistance developing to Primaquine?
So far, resistance to Primaquine’s hypnozoite‑clearing activity is rare. However, mutations associated with reduced drug susceptibility have been documented in the pvmdr1 gene, underscoring the need for continuous molecular surveillance.
What role does the WHO play in Primaquine deployment?
The WHO issues global treatment guidelines, recommends routine G6PD testing before Primaquine use, and maintains a safety database that tracks adverse events worldwide.
Hey folks, just wanted to point out that the G6PD testing is a real lifesaver when we think about rolling out Primaquine in community clinics.
Even in low‑resource settings, those sub‑$5 point‑of‑care kits have proven to be reliable.
It means we can protect millions of people without risking hemolysis.
And because the drug is cheap, you’re not breaking the bank for a 14‑day course.
Overall, it’s a win‑win for public health, especially in areas where malaria and dengue overlap.
First off, good job on highlighting the multi‑disease potential of Primaquine.
The lab data for dengue and Zika are promising, but we need real‑world efficacy studies before we start prescribing it en masse.
I’d add that any rollout must be paired with robust G6PD screening – otherwise we’ll see a surge in hemolytic events.
From a policy perspective, the cost‑effectiveness looks solid compared to newer, pricier options like Tafenoquine.
Still, let’s keep an eye on any emerging resistance markers in the pfcrt and pvmdr1 genes.
Bottom line: cautious optimism, but we can’t afford to be complacent.
Ever notice how every time a “new use” for an old drug comes out, the pharma giants rush to market it without telling us the full story?
They love to hype the cross‑protection against viruses while quietly pushing the cheap, unpatented version that keeps them in control of the supply chain.
And that G6PD test? It’s conveniently priced low now, but you can bet the next version will be locked behind a proprietary platform.
Bottom line, don’t be fooled by glossy press releases – there’s always a hidden agenda.
Stay skeptical and demand transparency.
While the article does a great job explaining the mechanism, there are a few minor errors that need correcting.
For instance, the phrase “point‑of‑care” should be hyphenated consistently throughout the text.
Also, “cost (per treatment)” in the table could be formatted as “Cost per treatment” for clarity.
These nit‑picks aside, the scientific content is solid and the references are on point.
Overall, a well‑written piece with just a few typographic hiccups.
Wow, this drug is a real game‑changer.
Super exciting to see a single pill potentially tackling malaria, dengue, Zika, and even chikungunya!
It’s like the Swiss‑army knife of infectious disease control.
With the low price tag and the ability to use existing supply chains, this could make a massive dent in global morbidity.
Let’s keep pushing for wider G6PD screening so everyone can benefit safely.
Cheering for the researchers and the communities that will see real impact.
Reading through the data on Primaquine, I’m struck by how a drug born in the 1940s can still surprise us with its versatility.
The fact that it can target dormant hypnozoites has already changed the game for vivax malaria eradication.
Now, the emerging evidence that it may also blunt dengue replication adds a whole new dimension to its utility.
If we can demonstrate consistent viral load reduction in clinical trials, we could see a paradigm shift where antimalarials double as antiviral adjuncts.
What’s even more compelling is the cost factor – a two‑dollar regimen compared to the hundreds of dollars for newer antivirals.
This affordability could democratize access in low‑income regions where dengue and Zika are endemic.
However, the shadow of G6PD deficiency looms large, reminding us that safety can’t be an afterthought.
The rapid point‑of‑care tests are a technological marvel, yet their deployment still requires training and supply chain logistics.
I also worry about the potential for resistance, especially as we start using Primaquine beyond its original indication.
Genetic monitoring of pfcrt and pvmdr1 mutations should become a routine part of any widescale program.
From an ecological perspective, reducing viral loads in humans might also decrease transmission intensity by the Aedes vectors.
That could translate to fewer outbreak cycles and lower healthcare burdens overall.
Yet, we must remain vigilant about possible off‑target effects, especially in pregnant women where Zika poses a teratogenic threat.
Balancing the benefits against the risks will require nuanced guidelines that incorporate local G6PD prevalence data.
In the end, Primaquine exemplifies how repurposing old drugs can breathe new life into public health strategies, a lesson we should carry forward.
Let’s champion collaborative research, equitable drug distribution, and robust safety monitoring – the future looks hopeful! 😊
Oh please, another “miracle pill” narrative. 🙄 History is full of overhyped drugs that never lived up to the hype, and Primaquine is no exception.
Sure, it’s cheap, but cheap often means compromised safety, especially for the millions of G6PD‑deficient people worldwide.
Why are we so quick to glorify a single molecule when comprehensive vector control and vaccine development are the real solutions?
Don’t get me wrong, I love a good repurposing story, but this feels like a PR stunt more than a scientific breakthrough.
Let’s keep the hype in check.
Honestly, this kind of defeatist talk just undermines our own country’s ability to lead in global health.
We have the manufacturing capacity to produce Primaquine at scale, and we can set the standards for safe G6PD testing.
If we let foreign critics dictate the narrative, we’ll lose our competitive edge.
Time to stand up, fund more trials, and prove the world that our approach works.
The focus should be on safety, not on bragging rights.
Even if we have capacity, deploying a drug without proper screening can cause harm.
Let’s prioritize patient health above national pride.
You’re absolutely right; safety must come first.
Implementing robust G6PD testing protocols alongside any Primaquine distribution ensures we protect vulnerable patients.
Collaboration between health ministries, NGOs, and local clinics can make this happen efficiently.
Let’s keep the conversation constructive and work toward solutions that safeguard everyone.
So much talk, and still no action – the clock is ticking.