SSRI and NSAID Risk Calculator
Assess Your GI Bleeding Risk
This tool estimates your risk of gastrointestinal bleeding when taking both SSRIs and NSAIDs together. It's not a medical diagnosis but helps you have important conversations with your doctor.
Combining SSRIs and NSAIDs might seem harmless-after all, millions of people take antidepressants for depression and over-the-counter painkillers for headaches or arthritis. But this everyday combination carries a hidden danger: a sharp rise in life-threatening gastrointestinal bleeding. It’s not rare. It’s not theoretical. And most people, including many doctors, don’t know about it.
Why This Combo Is Dangerously Common
About 1 in 8 U.S. adults takes an SSRI like sertraline, fluoxetine, or escitalopram. Nearly 1 in 6 regularly uses an NSAID like ibuprofen, naproxen, or diclofenac. That means over 30 million Americans are taking both. And when you put them together, the risk of bleeding in the stomach or intestines jumps by 75% compared to using NSAIDs alone. This isn’t just a small increase. It’s a multiplicative effect. NSAIDs alone raise GI bleeding risk 2 to 4 times. SSRIs alone raise it 1.5 to 2 times. Together? The risk isn’t just added-it’s multiplied. A 2022 meta-analysis of over 1.2 million patients confirmed this: the odds ratio was 1.75. That’s not a fluke. It’s consistent across studies, age groups, and even after adjusting for other risk factors like age or prior ulcers.How SSRIs and NSAIDs Work Together to Cause Bleeding
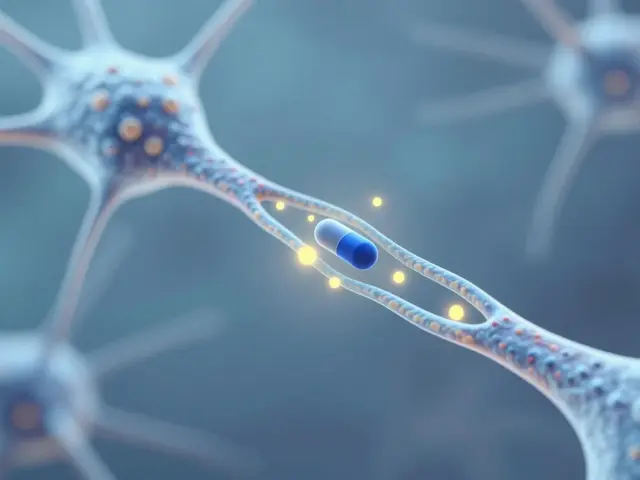
The problem isn’t just one drug-it’s two separate mechanisms that crash into each other. NSAIDs damage the stomach lining directly. They block prostaglandins, which are natural compounds that protect the gut and help maintain blood flow to the mucosa. Without them, the stomach becomes vulnerable to acid and inflammation. Over time, this can lead to ulcers. SSRIs do something different but just as dangerous. They block serotonin reuptake in the brain to improve mood-but they also block it in platelets. Platelets need serotonin to stick together and form clots. When serotonin is low in platelets, they can’t do their job. Even a minor tear in the stomach lining can’t seal properly. The result? Bleeding that doesn’t stop. Think of it like this: NSAIDs make the stomach lining fragile. SSRIs make your blood less able to clot. Put them together, and even a small irritation can turn into a serious bleed.Not All NSAIDs Are Created Equal
If you’re on an SSRI and need pain relief, not all NSAIDs are equally risky. Some are worse than others. Naproxen and diclofenac carry the highest bleeding risk among non-selective NSAIDs. Ibuprofen is slightly safer, but still dangerous when paired with an SSRI. Celecoxib, a COX-2 inhibitor, has a much lower risk-close to that of a placebo. One study found its odds ratio for bleeding was just 1.16 when used alone, compared to 1.8-2.5 for naproxen. But here’s the catch: even celecoxib isn’t risk-free when combined with an SSRI. The 75% increased risk still applies. So switching from naproxen to celecoxib helps-but it doesn’t eliminate the danger.Acetaminophen: The Safer Alternative
If you’re on an SSRI and need pain relief, acetaminophen (also called paracetamol) is your best bet. Unlike NSAIDs, it doesn’t affect prostaglandins or platelets. It doesn’t irritate the stomach lining. And it doesn’t interfere with serotonin in platelets. Multiple studies, including a 2023 meta-analysis of over a million patients, show no increased bleeding risk when acetaminophen is used with SSRIs. That’s not a small difference-it’s a complete absence of risk. Many patients don’t know this. One Reddit user wrote: “I was on sertraline and took ibuprofen every day for my back pain. I ended up in the ER with a bleeding ulcer. No one ever told me it was dangerous.” Switching to acetaminophen isn’t just safer-it’s often just as effective for headaches, muscle aches, and joint pain. It’s not a miracle drug for severe inflammation, but for most everyday discomfort, it’s the clear choice.
Who’s at the Highest Risk?
Not everyone on this combo will bleed. But some people are far more vulnerable:- People over 65
- Those with a history of ulcers or GI bleeding
- Anyone taking low-dose aspirin, warfarin, or other blood thinners
- Patients on high-dose NSAIDs (more than 1,200 mg of ibuprofen daily)
- Those who’ve been on SSRIs for more than 90 days
Proton Pump Inhibitors (PPIs) Can Help-but They’re Not a Fix
Many doctors prescribe a PPI like omeprazole or pantoprazole along with SSRIs and NSAIDs. And yes, PPIs reduce bleeding risk by about 70%. That sounds good. But here’s the problem: PPIs don’t fix the platelet issue caused by SSRIs. They only protect the stomach lining. A 2017 Lancet study showed that in patients taking both SSRIs and NSAIDs, PPIs dropped the annual bleeding rate from 1.5% to 0.5%. That’s meaningful-but it still means 1 in 200 people will bleed each year. And PPIs aren’t harmless. Long-term use is linked to kidney problems, bone fractures, and nutrient deficiencies. The best approach? Avoid the combo entirely. If you can’t, use the lowest possible NSAID dose for the shortest time. And always consider acetaminophen first.What Patients Are Saying
Patient experiences reveal a pattern: surprise and regret. On Drugs.com, 28% of users on SSRI-NSAID combos reported GI side effects. 12% specifically mentioned bleeding. One woman wrote: “I was on fluoxetine and naproxen for years. I started vomiting blood and didn’t know why. My doctor said it was ‘just stress.’ I spent three days in the hospital.” On Reddit, 68% of users in threads about this interaction said they had no idea it was dangerous. Many said their doctors never mentioned it. That’s not negligence-it’s ignorance. And it’s widespread. The good news? Patients who switched to acetaminophen reported zero GI issues. “My doctor switched me from naproxen to Tylenol when I started sertraline,” one user said. “No problems in two years. Why didn’t anyone tell me this before?”What Doctors Should Do
This isn’t just a patient problem. It’s a system problem. A 2021 study found that in 12 primary care clinics, 28% of patients were prescribed SSRIs and NSAIDs together. After a simple education program for clinicians, that number dropped to 9% in six months. Here’s what works:- Screen every patient on SSRIs: “Are you taking any painkillers regularly?”
- Never assume NSAIDs are safe just because they’re OTC.
- Recommend acetaminophen as the first-line pain reliever for SSRI users.
- If NSAIDs are absolutely necessary, use the lowest effective dose for the shortest time.
- Prescribe a PPI only if NSAIDs can’t be avoided-and monitor for long-term side effects.
- Document the interaction clearly in the EHR. Alerts reduce bleeding events by 32%.

The Bigger Picture: Why This Keeps Happening
The FDA required warning labels on SSRIs in 2019. The EMA recommended risk assessments in 2021. Yet, the combination remains common. Why? Because it’s invisible. Patients don’t connect their stomach pain to their antidepressant. Doctors don’t ask about OTC painkillers. Pharmacies don’t flag it. The system is designed for silos: one provider prescribes the SSRI, another prescribes the NSAID, and no one sees the full picture. The economic cost is staggering. In 2022, U.S. healthcare spending on SSRI-NSAID-related bleeding hit $1.2 billion-mostly from hospitalizations and ER visits. That’s not just money. It’s lives disrupted, families stressed, and preventable trauma.What’s Next? Safer Options Are Coming
Research is moving fast. Vortioxetine, a newer antidepressant, showed 40% less bleeding risk than traditional SSRIs in a 2022 trial. Lumateperone, a serotonin modulator, is being tested for depression without platelet effects. Both could be game-changers. New tools like the GI-BLEED risk calculator (now in Epic EHR systems) use 12 variables-including genetics, drug types, and age-to give personalized risk scores. Accuracy? 89%. By 2030, experts predict a 60% drop in inappropriate SSRI-NSAID combinations thanks to better alerts, patient education, and safer alternatives.What You Can Do Today
If you’re on an SSRI:- Ask your doctor: “Am I taking any NSAIDs? Are they necessary?”
- Replace ibuprofen, naproxen, or diclofenac with acetaminophen for pain.
- Don’t assume aspirin is safe-it’s even riskier with SSRIs.
- Know the signs of GI bleeding: black or tarry stools, vomiting blood, sudden dizziness, or severe abdominal pain.
- Don’t wait for symptoms. If you’re on both drugs, talk to your doctor now.
- Ask about OTC meds in every visit.
- Prescribe acetaminophen first for SSRI patients needing pain relief.
- Use EHR alerts. Document the interaction. Educate your patients.
Can I take ibuprofen with sertraline?
Taking ibuprofen with sertraline increases your risk of gastrointestinal bleeding by about 75% compared to taking ibuprofen alone. While it’s not absolutely forbidden, it’s not safe either. The combination affects both your stomach lining and your blood’s ability to clot. If you need pain relief, switch to acetaminophen (Tylenol) instead-it doesn’t carry this risk.
Do all SSRIs have the same bleeding risk?
Not all SSRIs carry equal risk. Drugs like paroxetine and fluoxetine strongly inhibit serotonin reuptake in platelets, making them higher risk. Sertraline and citalopram have weaker effects and may be slightly safer-but the difference isn’t enough to rely on. The safest approach is to avoid NSAIDs entirely, regardless of which SSRI you’re on.
Is celecoxib safer than other NSAIDs with SSRIs?
Yes, celecoxib carries a lower risk of GI bleeding than non-selective NSAIDs like naproxen or diclofenac. Studies show its bleeding risk is close to baseline when used alone. But when combined with an SSRI, the 75% increased risk still applies. It’s safer-but not safe. Acetaminophen remains the best alternative.
Can PPIs prevent bleeding from SSRIs and NSAIDs?
PPIs like omeprazole reduce bleeding risk by about 70% by protecting the stomach lining. But they don’t fix the platelet problem caused by SSRIs. That means bleeding can still happen, especially if you’re on high-dose NSAIDs or have other risk factors. PPIs are a safety net, not a solution. Avoiding the combo altogether is better.
What should I do if I’m already taking both?
Don’t stop either medication suddenly. Talk to your doctor. Ask if you can switch your NSAID to acetaminophen. If you need the NSAID for a condition like arthritis, ask if the dose can be lowered or if you can take it only as needed. Consider a PPI only if the NSAID can’t be avoided. And watch for signs of bleeding: black stools, vomiting blood, or sudden weakness.
Is this risk higher in older adults?
Yes. People over 65 are at much higher risk because their stomach lining is thinner, their kidneys process drugs slower, and they’re more likely to have other conditions or medications that add to the risk. If you’re over 65 and on both an SSRI and an NSAID, your risk of bleeding is among the highest. Switching to acetaminophen is strongly recommended.
Can I take aspirin with an SSRI?
Taking low-dose aspirin with an SSRI is one of the riskiest combinations possible. Aspirin also inhibits platelets, and when combined with an SSRI, it creates a double hit on clotting. Studies show this combo can increase bleeding risk more than 12-fold compared to not taking either. If you’re on an SSRI and need aspirin for heart protection, talk to your doctor about alternatives like clopidogrel or whether the aspirin is truly necessary.
Now I use Tylenol. Zero issues. Why didn't anyone tell me this was a thing? 😔
Who profits? The hospital. The ER. The GI specialist. The PPI manufacturer. The algorithm that recommends ‘commonly prescribed together’ in the EHR.
We’re not patients. We’re data points with bleeding ulcers.
And guess what? I switched to paracetamol. No drama. No panic. Just… care.
Also, NSAID class matters. COX-2 selectivity reduces GI toxicity, but cardiovascular risk? That’s the other side of the coin. This is a risk-benefit calculus, not a binary good/bad.
Don’t overcomplicate it. Ask your doctor. Switch. Done.
But you? You read this. You know. Now you’re dangerous. Because awareness is the first act of rebellion.
Simple question: ‘What OTC meds are you using?’ Could’ve saved his life.
Maybe the answer isn’t more pills. Maybe it’s less fear. Less noise. Just… acetaminophen. Simple. Safe. Silent hero.
My doctor said, ‘We should’ve caught this.’
Now I use Tylenol. My back still hurts. But I’m alive. And I’m telling everyone I know. This needs to be shouted from rooftops. 🌍❤️
Doctors, patients, pharmacists-we all need to stop treating OTC like it’s harmless. It’s not. It’s medicine. And medicine has consequences.
Thank you for writing this. I’m sharing it with my mom.