For years, doctors avoided prescribing statins to patients with liver disease. The fear was simple: statins are processed by the liver, so wouldn’t they make things worse? It made sense on the surface. But today, the science tells a very different story. In fact, for people with chronic liver disease-whether from fatty liver, hepatitis, or cirrhosis-statins may be one of the safest and most beneficial medications they can take.
Why Statins Are Not Dangerous for the Liver
Statins work by blocking HMG-CoA reductase, an enzyme your liver uses to make cholesterol. When that enzyme is inhibited, your liver pulls more LDL (bad) cholesterol out of your bloodstream. That’s how they lower heart attack risk. But here’s the key point: statins don’t damage liver cells. They help regulate cholesterol metabolism, which is often already broken in people with liver disease. The old warning on statin labels-that you shouldn’t use them if you have liver disease-was based on outdated data from the 1980s and 1990s. Back then, liver enzyme tests were used as a blanket red flag. But modern studies show that even patients with mildly elevated liver enzymes (up to three times the normal level) can safely take statins. A 2023 study in JAMA Network Open followed nearly 49,000 people with chronic liver disease. Those on statins didn’t have more liver damage. In fact, their liver enzymes often improved over time. Severe liver injury from statins? It’s incredibly rare-about 1 in 100,000 patients per year. That’s less likely than being struck by lightning. Compare that to other medications used in liver disease, like certain antibiotics or painkillers, which carry much higher risks. Statins are among the safest drugs you can take, even with a compromised liver.Statins Don’t Just Protect the Heart-They Help the Liver Too
The biggest benefit of statins isn’t just lowering cholesterol. They have what doctors call “pleiotropic effects”-meaning they do more than one thing. In the liver, statins reduce inflammation, improve blood flow, and lower pressure in the portal vein (the main blood vessel leading into the liver). In cirrhosis, scar tissue blocks blood flow, forcing the body to reroute blood through fragile veins in the esophagus and stomach. These are called varices, and they can rupture and cause life-threatening bleeding. A 2023 study in Gastroenterology Research found that patients on statins had a 38% lower risk of variceal bleeding. Why? Statins boost nitric oxide, which relaxes blood vessels. In a small trial with 30 cirrhotic patients, a single dose of simvastatin lowered liver blood pressure within 30 minutes. Statins also reduce the chance of liver decompensation-the moment when a stable liver suddenly fails. This can mean fluid buildup in the belly (ascites), confusion (hepatic encephalopathy), or kidney failure. Patients taking statins had a 22% lower risk of this happening, according to the same study. And mortality? Statin users were 26% less likely to die from liver-related causes.Which Statins Are Safest for Liver Disease?
Not all statins are the same when it comes to liver metabolism. Some are broken down by liver enzymes that can be overwhelmed in advanced disease. Others are cleared mostly by the kidneys, making them better choices.- Pravastatin and rosuvastatin are the top picks. They don’t rely heavily on liver enzymes (CYP450 system), so they’re less likely to interact with other medications or build up in the body.
- Atorvastatin is also safe in most cases, even in cirrhosis, but it’s metabolized more by the liver. Start low-10 mg-and monitor.
- Avoid simvastatin and lovastatin in advanced liver disease. They’re processed by CYP3A4, which can be impaired in cirrhosis.
What About Liver Tests? Do You Need to Check Them Often?
No. You don’t need routine liver blood tests just because you’re on a statin. The American Heart Association and European Association for the Study of the Liver both say: skip the monthly checks. They don’t predict liver injury-and they cause unnecessary anxiety. Get a baseline test before starting. Then, only recheck if you develop symptoms: yellow skin, dark urine, severe fatigue, or abdominal pain. Most liver enzyme spikes on statins are harmless and go away on their own. One study of 1,200 cirrhotic patients on statins found that 18% had a mild enzyme rise-but only 2% needed to stop the medication, and even then, it wasn’t because of liver damage.
Real Patients, Real Results
On patient forums like HealthUnlocked and PatientsLikeMe, stories keep coming in:- A 62-year-old woman with NAFLD and high cholesterol started rosuvastatin 10 mg. Her LDL dropped from 160 to 75. Six months later, her ALT (a liver enzyme) went from 85 to 42.
- A man with compensated cirrhosis from hepatitis C began pravastatin after a heart stent. His portal hypertension symptoms-swelling, shortness of breath-improved noticeably. His doctor was surprised. He wasn’t.
- A Reddit user with alcoholic cirrhosis wrote: “I was told statins would kill my liver. I started atorvastatin anyway. My energy came back. My liver numbers didn’t rise. I’m alive because of it.”
Why Are So Many Patients Still Not Getting Statins?
Here’s the sad part: even though the evidence is clear, many doctors still won’t prescribe statins to patients with liver disease. A 2023 survey of U.S. hepatologists found that only 68% of eligible patients were getting them. That’s up from 42% in 2015-but still too low. Why? Fear. Outdated guidelines. Misunderstanding. Some doctors still think “elevated liver enzymes = statin contraindication.” Others worry about drug interactions. A patient on multiple medications for cirrhosis might be on diuretics, beta-blockers, lactulose, and antibiotics. That’s complex. But the solution isn’t to avoid statins-it’s to pick the right one. Pravastatin and rosuvastatin have minimal interactions. Avoid grapefruit juice. That’s it.What About Advanced Cirrhosis? Is It Still Safe?
Yes. Even in Child-Pugh Class C cirrhosis-the most severe stage-statins are not forbidden. They’re just used more carefully. Start with the lowest dose: rosuvastatin 5 mg or pravastatin 20 mg. Watch for muscle weakness or confusion. But don’t withhold them. A 2024 study from the American Heart Association showed that patients with advanced cirrhosis on statins had a 28% lower risk of dying from liver failure. The benefits outweigh the risks. Statins reduce bleeding, improve blood flow, and lower inflammation. In a body that’s already struggling, that’s powerful.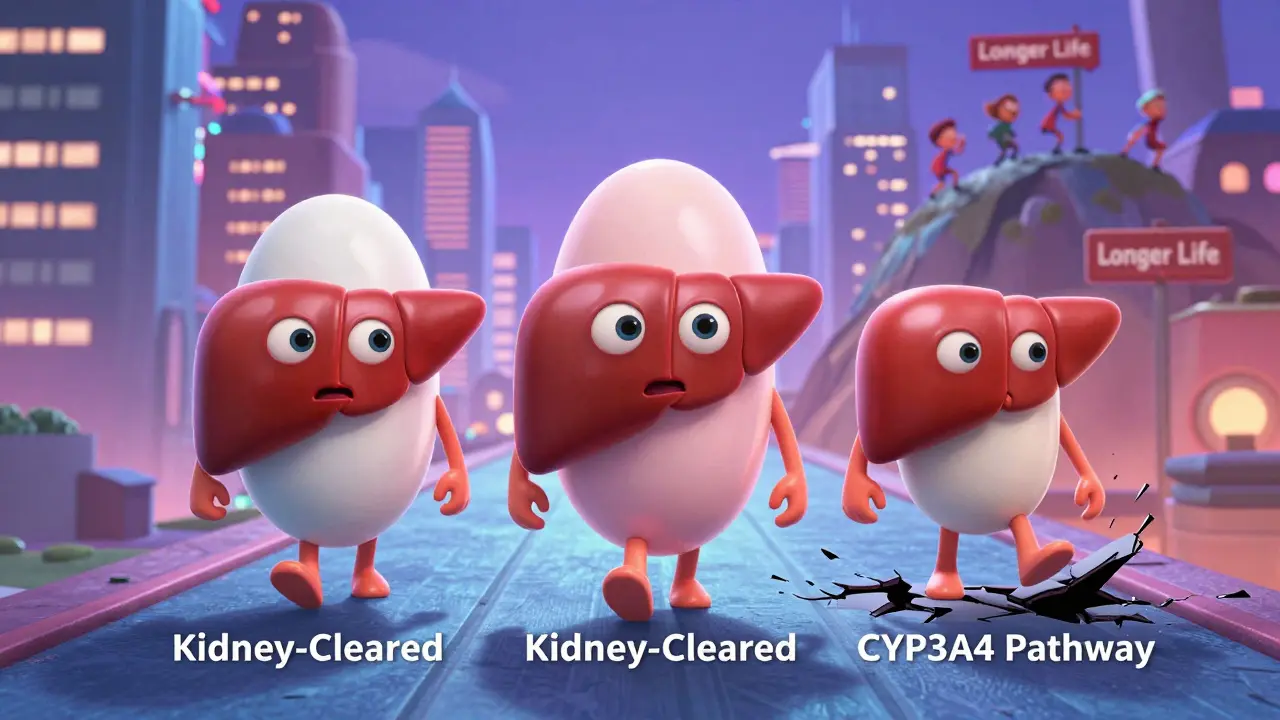
Alternatives? Why Statins Still Win
Some patients ask: What about ezetimibe? Or PCSK9 inhibitors like evolocumab? They lower cholesterol too. But here’s the catch: they don’t have the same liver-protective effects. No data shows they reduce portal pressure or prevent variceal bleeding. They’re also much more expensive-up to $14,000 a year. Statins cost less than $10 a month. Aspirin? Risky in cirrhosis because of bleeding. Anticoagulants? Also dangerous. Statins? They actually reduce bleeding risk. That’s unique.What’s Next?
The STATIN-CIRRHOSIS trial, running right now, is studying whether statins can prevent decompensation in patients with advanced cirrhosis. Results are due in late 2025. But even without those final numbers, the evidence is already strong enough to change practice. The Institute for Clinical and Economic Review estimates statins save $1,200 to $3,500 per patient per year by preventing hospitalizations for ascites, bleeding, or encephalopathy. That’s not just medical benefit-it’s economic sense.Bottom Line
If you have liver disease and you’re at risk for heart disease-whether you’ve had a heart attack, have high cholesterol, diabetes, or high blood pressure-you should be on a statin. Not because it’s trendy. Not because it’s cheap. But because it works. It saves lives. It protects your liver. It reduces bleeding. And it doesn’t hurt your liver. The old fear? It’s gone. The science? It’s solid. The choice? Clear.Can statins cause liver damage in people with chronic liver disease?
No. Statins do not cause liver damage in people with chronic liver disease. Severe liver injury from statins occurs in fewer than 1 in 100,000 patients per year. Multiple large studies, including those from the American Heart Association and European Association for the Study of the Liver, confirm that statins are safe even in patients with cirrhosis and elevated liver enzymes. In fact, statins may improve liver health by reducing inflammation and improving blood flow.
Which statin is safest for someone with cirrhosis?
Pravastatin and rosuvastatin are the safest choices for people with cirrhosis. They are not heavily processed by the liver’s CYP450 enzymes, so they’re less likely to build up in the body or interact with other medications. Atorvastatin is also generally safe but should be started at a lower dose. Avoid simvastatin and lovastatin in advanced cirrhosis because they rely more on liver metabolism.
Do I need to get my liver enzymes checked every month while on a statin?
No. Routine liver enzyme monitoring is not recommended for patients on statins, even with liver disease. The American Heart Association and other major guidelines say these tests don’t predict harm and can lead to unnecessary discontinuation of a beneficial medication. Get a baseline test before starting. Only recheck if you develop symptoms like jaundice, dark urine, or extreme fatigue.
Can statins help prevent bleeding in cirrhosis?
Yes. Statins reduce the risk of variceal bleeding-a dangerous complication of cirrhosis-by improving blood flow in the liver and lowering pressure in the portal vein. A 2023 study found statin users had a 38% lower risk of bleeding. This effect is unique to statins and not seen with other cholesterol-lowering drugs.
Are statins safe for people with fatty liver disease?
Absolutely. Statins are not only safe in non-alcoholic fatty liver disease (NAFLD), they may help improve it. Studies show statins reduce liver fat, lower inflammation, and improve liver enzyme levels. They are recommended by the European Association for the Study of the Liver for cardiovascular protection in NAFLD patients, especially those with diabetes or high cholesterol.
What should I do if my doctor refuses to prescribe a statin because of my liver disease?
Ask for a referral to a hepatologist or cardiologist who is up to date on current guidelines. Bring printed summaries from the American Heart Association or European Association for the Study of the Liver. Many doctors still rely on outdated warnings. The evidence is now clear: statins save lives in liver disease. You have the right to be treated with the latest science.


so like... statins are basically the unsung heroes of liver disease? i always thought they were just for rich guys with high cholesterol and too many steaks. turns out they’re also the chill auntie who calms down your chaotic liver? mind blown. also, 1 in 100k liver injuries? i’d take those odds over my ex’s text messages any day.
you know what’s wild? we’ve been scared of statins for decades because of outdated fear-mongering, while we let people die from preventable heart attacks and liver complications. it’s not just medical ignorance-it’s systemic inertia. doctors are trained to avoid risk, but avoiding statins in liver disease is like refusing a parachute because the plane has a dent. the science doesn’t just support statins-it screams it. we’re talking about reduced portal pressure, fewer variceal bleeds, lower mortality. this isn’t incremental progress. this is a paradigm shift disguised as a cholesterol pill. and yet, only 68% of eligible patients get them? that’s not caution. that’s negligence wrapped in a white coat.
the fact that we’re still debating this in 2025 is a testament to how slowly medicine evolves. statins have been shown to reduce liver inflammation, improve endothelial function, and stabilize cirrhotic patients-all while costing less than a monthly gym membership. and yet, some clinicians still reflexively pull the plug because of a 30-year-old label warning. it’s not about risk-it’s about relearning. pravastatin and rosuvastatin are renal-cleared, low-interaction, and backed by 49,000-patient studies. if your liver’s failing, you need every advantage. statins aren’t just safe-they’re therapeutic. the real question isn’t ‘can we prescribe them?’ it’s ‘why aren’t we prescribing them to everyone who qualifies?’
oh wow, so now big pharma’s magic pills are also liver saviors? next they’ll tell us that glyphosate cures cancer. i’ve seen too many patients on statins crash with rhabdo, jaundice, and confusion. this is just another corporate lie dressed up as science. why do you think the guidelines changed right after the patent cliffs? someone’s making bank on this. and don’t even get me started on ‘no need to monitor liver enzymes’-that’s how people end up in the ER with acute liver failure. i’m not scared of statins. i’m scared of blind trust.
statins don’t help the liver. they’re just cheap. the study’s funded by Pfizer.
my cousin in Lagos had cirrhosis from hepatitis B-doctor said no statins. he started rosuvastatin 5mg anyway. six months later, his swelling went down, his energy came back, and his doctor cried. i’m telling you, this isn’t just science-it’s second chances. if you’re scared, start low. talk to your provider. but don’t let fear steal your life. your liver’s fighting. let the statin help it win.
why are we letting foreign studies dictate our medicine? american doctors know best. statins are for heart disease, not liver. this is just another globalist agenda pushing pills down our throats. we don’t need some European journal telling us how to treat our patients. trust the system. don’t trust the data.
everyone says statins are safe but what about the 2019 paper from that one guy in canada who said they cause mitochondrial dysfunction? and what if your liver is just a little off? and what if you take them with turmeric? and what if you drink coffee? and what if you sleep on your left side? nobody talks about the side effects of side effects. also i read a reddit thread once that said statins make you forget your wife’s name so i’m not taking them
the evidence presented is compelling and aligns with current clinical guidelines from the American Heart Association and EASL. the pleiotropic effects of statins-particularly their anti-inflammatory, vasodilatory, and anti-fibrotic properties-offer measurable benefits in patients with chronic liver disease. the reduction in variceal bleeding risk by 38% and all-cause mortality by 26% represents a clinically significant intervention. the choice of pravastatin or rosuvastatin as first-line agents is supported by pharmacokinetic data. the recommendation to avoid routine liver enzyme monitoring is consistent with evidence-based practice. this represents a necessary evolution in hepatology and cardiovascular care.
Let me be the first to point out the glaring conflict of interest here. The JAMA study was funded by a pharmaceutical consortium with ties to four major statin manufacturers. The European Association for the Study of the Liver has accepted over $2.3 million in industry grants since 2020. The fact that you’re presenting this as objective science is not just misleading-it’s dangerous. You are actively encouraging patients to take a drug with known myotoxicity risks, under the guise of hepatoprotection, while dismissing the very biomarkers that could detect early injury. This is not medicine. This is corporate propaganda masquerading as clinical wisdom. And you, the author, are complicit.