Antacids: What They Are, How They Work, and When to Use Them
When your chest burns after eating or your stomach feels like it’s bubbling up, antacids, over-the-counter medications that neutralize stomach acid to relieve heartburn and indigestion. Also known as acid neutralizers, they’re often the first thing people reach for when discomfort hits. They work fast—usually within minutes—by counteracting excess acid in your stomach. But they don’t fix the root problem. If you’re using them daily, you’re treating the symptom, not the cause.
Antacids come in many forms: chewable tablets, liquids, and even gels. Common ingredients include calcium carbonate, magnesium hydroxide, and aluminum hydroxide. Each has pros and cons. Calcium carbonate gives quick relief but can cause constipation or rebound acid production. Magnesium hydroxide works fast and can loosen stools, while aluminum hydroxide may cause constipation. Some products mix both to balance side effects. But here’s the catch: proton pump inhibitors, medications that reduce acid production at the source, not just neutralize it like omeprazole or esomeprazole, are better for frequent or long-term use. Antacids won’t heal an ulcer or stop chronic acid reflux—they just mask it.
People often confuse antacids with other acid-reducing drugs. heartburn, the burning sensation caused by stomach acid backing up into the esophagus can be triggered by spicy food, large meals, lying down after eating, or even stress. Antacids help with those sudden flares, but if it’s happening more than twice a week, you might be dealing with acid reflux, a condition where stomach acid regularly flows back into the esophagus. That’s when you need to look beyond antacids—maybe to lifestyle changes, prescription meds, or even testing for GERD.
And here’s something most don’t realize: antacids can interfere with other medications. They can block absorption of antibiotics, thyroid meds, iron pills, and even some antidepressants. Taking them at the same time as other drugs can make those drugs less effective. Always space them out by at least two hours. If you’re on multiple meds, check with your pharmacist before popping an antacid.
There’s no shame in using antacids for occasional relief. They’re safe for most people when used as directed. But if you’re relying on them week after week, you’re ignoring a signal your body is sending. The posts below cover real cases: how long-term acid suppression affects bone health, why some people get worse symptoms after stopping antacids, and what alternatives actually work. You’ll find clear advice on when to switch from antacids to something more effective—and when to talk to a doctor before it’s too late.
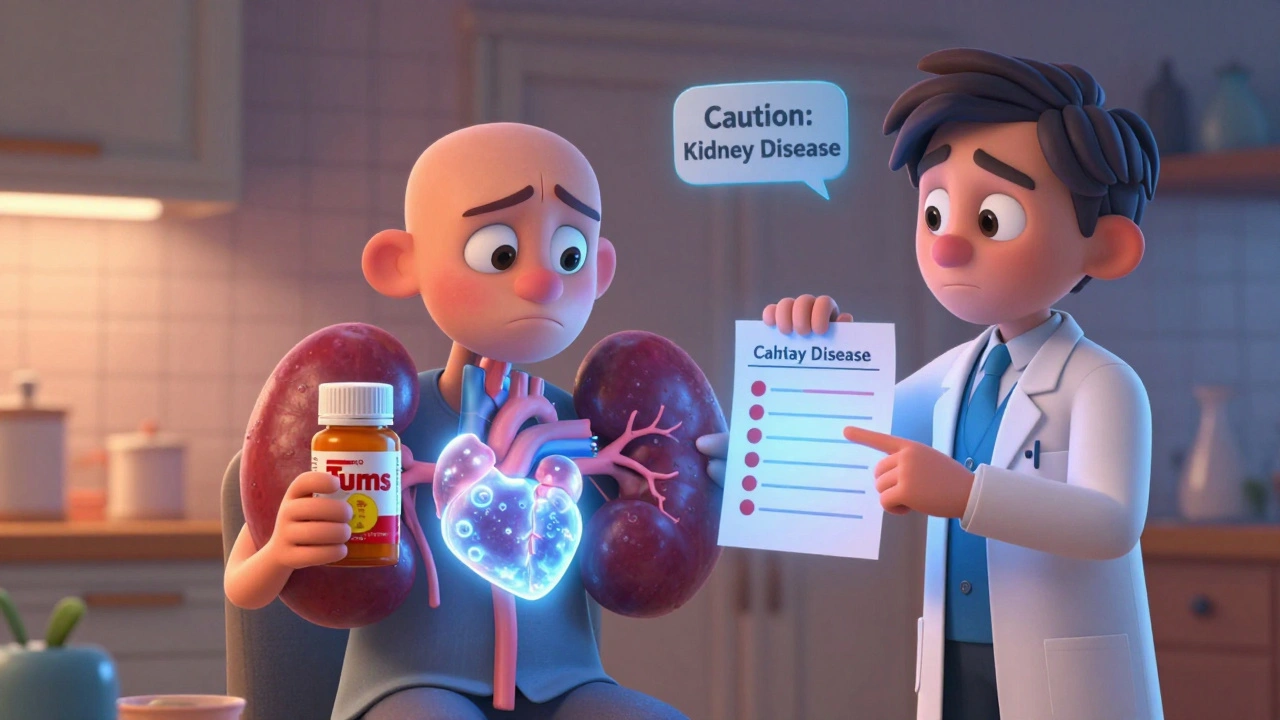
Antacids and Kidney Disease: What You Need to Know About Phosphate Binders and Risks
Antacids like Tums and Milk of Magnesia are common for heartburn, but for people with kidney disease, they can be dangerous. Learn how calcium, aluminum, and magnesium in these drugs affect phosphate levels, kidney function, and heart health.