Clopidogrel Effectiveness: How Well It Works and What Affects It
When your doctor prescribes clopidogrel, a prescription antiplatelet drug used to prevent blood clots in people with heart disease or after a stroke. Also known as Plavix, it’s one of the most common meds for keeping arteries clear after a heart attack or stent placement. But here’s the thing—not everyone responds the same way. Some people take it daily and stay protected. Others still end up with clots, even when they don’t miss a pill. Why? It’s not about willpower. It’s about biology, other meds, and genetics.
Aspirin, a widely used blood thinner often paired with clopidogrel is a common combo, but studies show mixing them doesn’t always mean better results—and can raise bleeding risk. Then there’s proton pump inhibitors, like omeprazole, used for heartburn. Some of these can block clopidogrel from working right. It’s not a myth—it’s in the science. If you’re on both, talk to your doctor. There are PPIs that don’t interfere, like pantoprazole, and switching might make all the difference.
Genetics play a big role too. About 30% of people have a gene variation that makes their body turn clopidogrel into its active form poorly. That’s called a poor metabolizer. It doesn’t mean the drug is weak—it means your body can’t use it the way it’s supposed to. Blood tests can find this, but most docs don’t order them unless someone has repeated clots. If you’ve had a stent and still had a problem, ask if genetic testing makes sense.
Other meds can mess with clopidogrel too. Antidepressants like fluoxetine, antifungals like fluconazole, and even some acid reflux drugs can get in the way. And if you’re on multiple pills for diabetes, high blood pressure, or cholesterol, the chances of an interaction go up. That’s why comorbidities, like diabetes or kidney disease matter. They don’t just add risk—they change how your body handles drugs.
Effectiveness isn’t just about whether it works—it’s about whether it works for you. Some people need a higher dose. Others need a different drug entirely, like ticagrelor or prasugrel. These newer antiplatelets work faster and more reliably, but they’re pricier and carry higher bleeding risks. It’s a trade-off.
And let’s not forget adherence. Half of all patients skip pills at some point, not because they’re careless, but because they forget, it’s expensive, or they feel fine and think they don’t need it anymore. But clopidogrel isn’t a cure—it’s insurance. Stop it too soon, and your risk spikes fast.
What you’ll find below are real, practical posts that dig into the details: how clopidogrel interacts with other meds, why side effects happen, what to do if it’s not working, and how to tell if you’re getting the most out of it. No fluff. Just what you need to know to stay safe and get results.
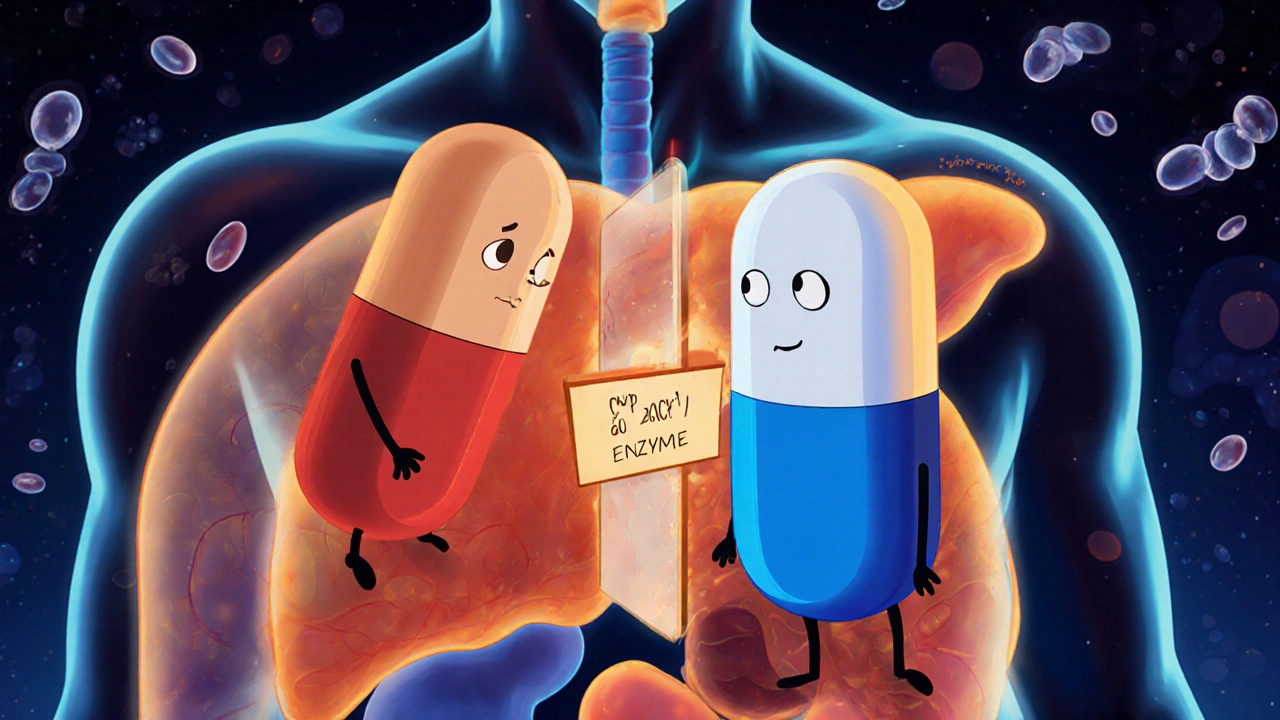
Omeprazole and Clopidogrel: What You Need to Know About CYP2C19 Inhibition
Omeprazole can reduce clopidogrel's effectiveness by blocking CYP2C19, the enzyme needed to activate it. Learn which PPIs are safer, how genetics play a role, and what alternatives exist.