G6PD deficiency: Risks, Triggers, and Managing Medication
When working with G6PD deficiency, a genetic enzyme disorder that reduces the body’s ability to protect red blood cells from oxidative damage. Also known as glucose‑6‑phosphate dehydrogenase deficiency, it primarily affects males because the responsible gene sits on the X chromosome. People with this condition can appear completely healthy until they encounter a trigger that overwhelms the weakened defense system, leading to sudden hemolysis. Understanding how the deficiency works is the first step toward avoiding painful episodes and staying on the right medication.
Key Considerations for Managing G6PD Deficiency
The root of the problem lies in the Glucose‑6‑Phosphate Dehydrogenase enzyme, the catalyst that fuels the pentose‑phosphate pathway and generates NADPH to keep red blood cells stable. When the enzyme’s activity drops, red cells can’t neutralize reactive oxygen species, making them vulnerable to breaking apart. This vulnerability is inherited in an X‑linked pattern, meaning mothers can pass the altered gene to sons and daughters, but symptoms show up most often in those with a single X chromosome. Recognizing the inheritance pattern helps families decide on newborn screening and informs doctors about potential risks before prescribing medication.
One of the most common clinical outcomes of the enzyme shortfall is hemolytic anemia, a condition where red blood cells rupture faster than the body can replace them. Symptoms range from mild fatigue and pale skin to severe jaundice and dark urine. The anemia can develop within hours of exposure to a trigger, so early detection is crucial. Lab tests usually show a rapid drop in hemoglobin and an increase in bilirubin, signaling that the red cells are being destroyed. Knowing these signs lets patients and clinicians act fast, often with supportive care and removal of the offending agent.
Oxidative stress, the imbalance between free radicals and the body’s ability to detoxify them is the underlying mechanism that drives hemolysis in G6PD deficiency. Foods like fava beans, certain infections, and a wide array of drugs can spike oxidative stress, overwhelming the limited NADPH supply. Even seemingly harmless over‑the‑counter products such as some pain relievers or cold remedies may carry hidden risks. The degree of stress depends on the specific trigger, the individual's enzyme activity level, and how long the exposure lasts. Monitoring diet and medication lists is a practical way to keep oxidative stress in check.
Because the condition is drug‑sensitive, the biggest challenge for patients is navigating the pharmacy aisle. Antibiotics such as sulfonamides, certain antimalarials, and some fluoroquinolones are classic red flags. Even common blood‑pressure combos like lisinopril‑HCTZ or beta‑blockers can cause problems in a subset of individuals. Our collection below breaks down the safety profile of many widely used medicines, from antihypertensives and antibiotics to pain relievers and cholesterol‑lowering agents. By reviewing these guides, you’ll know which drugs to avoid, which ones are generally safe, and how to discuss alternatives with your healthcare provider.
Armed with a clear picture of how the enzyme deficiency works, the inheritance pattern, and the triggers that spark oxidative stress, you’re ready to dive into the specific medication reviews. Below you’ll find practical, up‑to‑date information that helps you choose treatments without risking a hemolytic crisis. Let’s get into the details so you can stay safe and confident in managing your health.
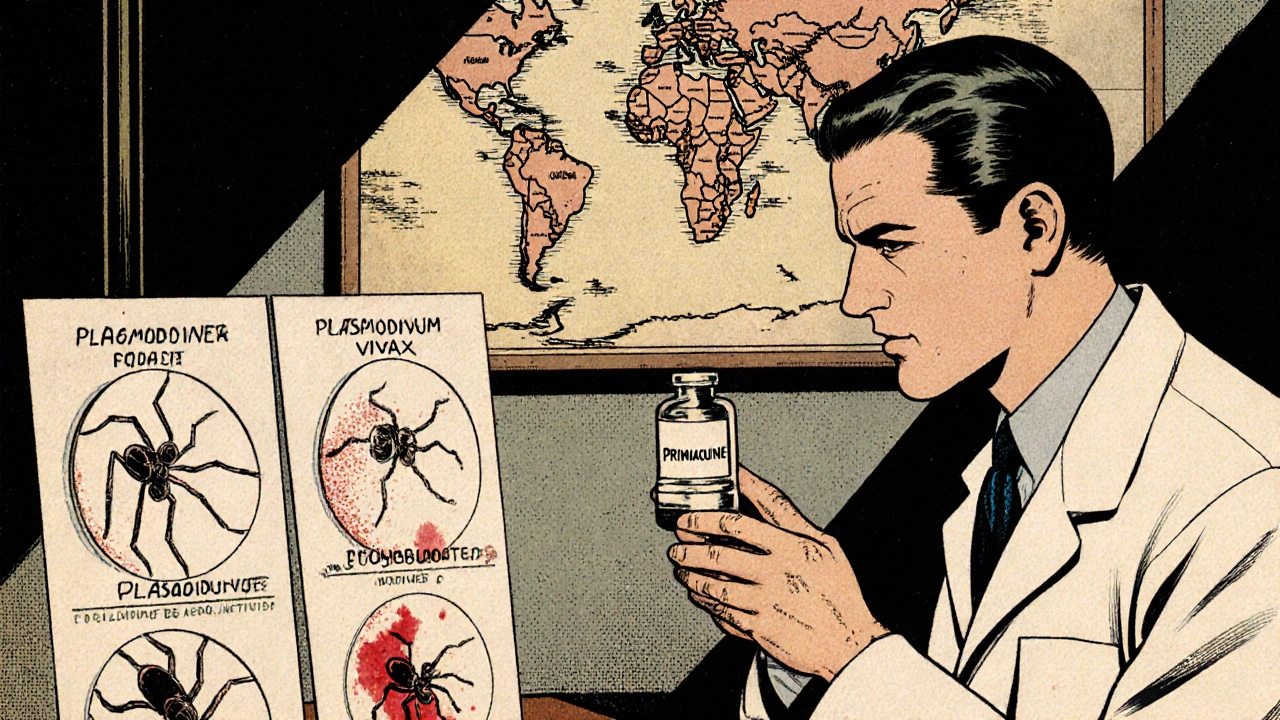
Primaquine’s Expanding Role Against Mosquito‑Borne Diseases
Explore how Primaquine, the malaria drug, is being studied to tackle other mosquito‑borne illnesses, its safety challenges, resistance concerns, and practical guidance for clinicians.