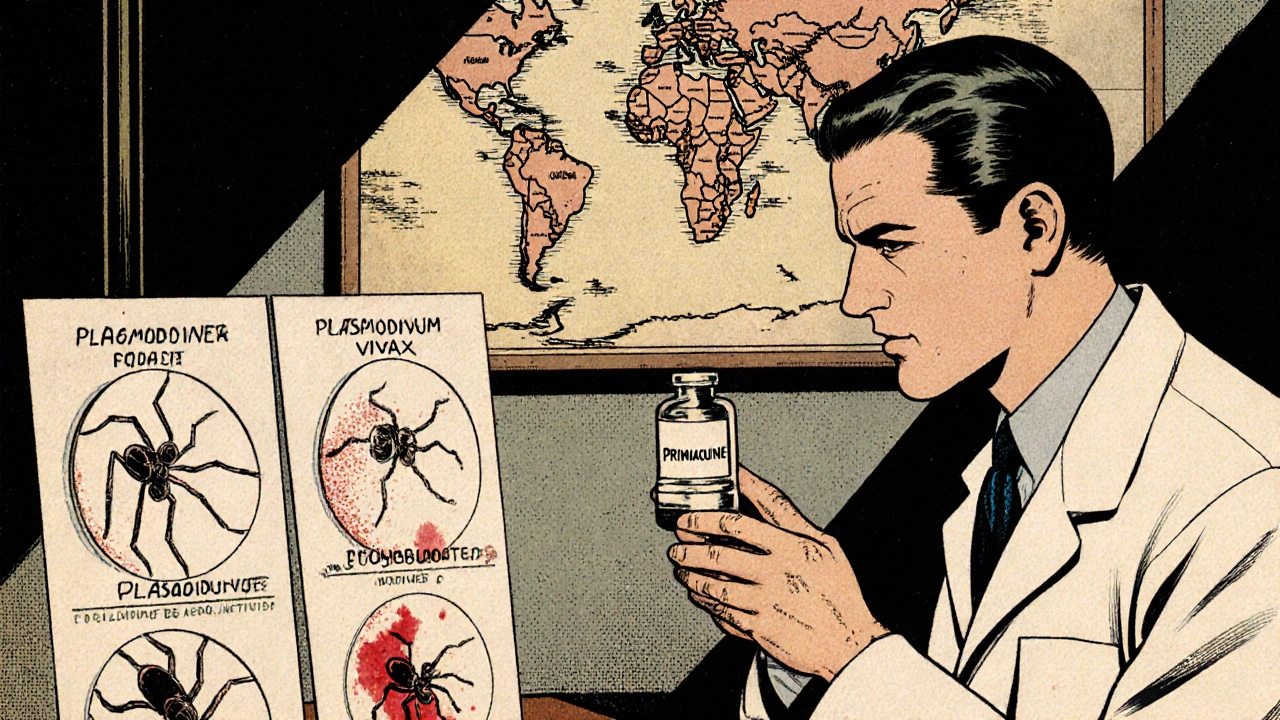
Primaquine – Everything You Need to Know
When you see Primaquine, an oral antimalarial that targets the liver stages of malaria parasites, also known as primaquine phosphate, you’re looking at a drug that does more than just treat a fever. It’s the only medication that can clear dormant hypnozoites, the hidden forms of malaria caused by Plasmodium vivax and P. ovale. Because of that, Primaquine is essential for both radical cure after infection and for preventing relapse in travelers.
Why Primaquine Matters in Modern Malaria Care
Primaquine belongs to the broader class of antimalarial drugs, medicines designed to stop malaria parasites from multiplying. Unlike many blood‑stage agents, it works deep in the liver, hitting the stages that other drugs miss. That makes it a key player in malaria prophylaxis, especially for people heading to regions where P. vivax is common. Health‑care providers often add a short course of Primaquine after a standard treatment to make sure the infection doesn’t come back months later.
But there’s a catch: Primaquine can cause hemolysis in patients with G6PD deficiency, a genetic enzyme disorder. The drug’s oxidative stress triggers red‑blood‑cell breakdown, which can be dangerous. That’s why a simple G6PD test is now a standard step before prescribing Primaquine. The test is quick, inexpensive, and can prevent serious complications.
Besides the safety check, dosing varies by indication. For radical cure of P. vivax or P. ovale, the typical adult regimen is 0.5 mg/kg daily for 14 days. For malaria prophylaxis, a lower daily dose (0.25 mg/kg) starts one to two days before entering the endemic area and continues for seven days after leaving. Pediatric dosing follows weight‑based charts, and renal or hepatic impairment may require adjustments. The drug is usually well tolerated; the most common side effects are mild gastrointestinal upset and a transient metallic taste.
In practice, clinicians often face questions like: “Can I take Primaquine while pregnant?” or “What if I’m breastfeeding?” The consensus is to avoid Primaquine during pregnancy because the fetus can’t process the drug safely. Breastfeeding mothers should wait until the infant is at least six months old, or discuss alternatives with their doctor. For travelers on a tight schedule, the short 14‑day regimen fits well with most vacation plans, and the prophylactic schedule aligns with typical travel itineraries.
When you combine Primaquine with other antimalarials—such as chloroquine or artemisinin‑based combos—it creates a comprehensive attack on the parasite: one drug clears the blood, the other wipes out the liver stash. This combination strategy is especially important in regions where resistance to single agents is rising. By covering both life‑cycle stages, the risk of treatment failure drops dramatically.
Beyond malaria, researchers are exploring Primaquine’s potential against other parasites, like certain helminths, though those uses remain experimental. The drug’s long half‑life—about six hours—means it stays in the system just long enough to do its job without causing accumulation in most patients.
Overall, Primaquine is a small tablet with a big impact. Whether you’re a traveler, a clinician, or a public‑health worker, understanding its role, safety checks, and proper dosing can make the difference between a one‑off infection and a lifelong freedom from relapse.
Below you’ll find a curated list of articles that dive deeper into dosing guides, safety considerations, drug comparisons, and real‑world tips for using Primaquine effectively. Keep reading to get the practical insights you need to make informed decisions about this essential antimalarial.
Primaquine’s Expanding Role Against Mosquito‑Borne Diseases
Explore how Primaquine, the malaria drug, is being studied to tackle other mosquito‑borne illnesses, its safety challenges, resistance concerns, and practical guidance for clinicians.