Understanding Functional Dyspepsia and Irritable Bowel Syndrome
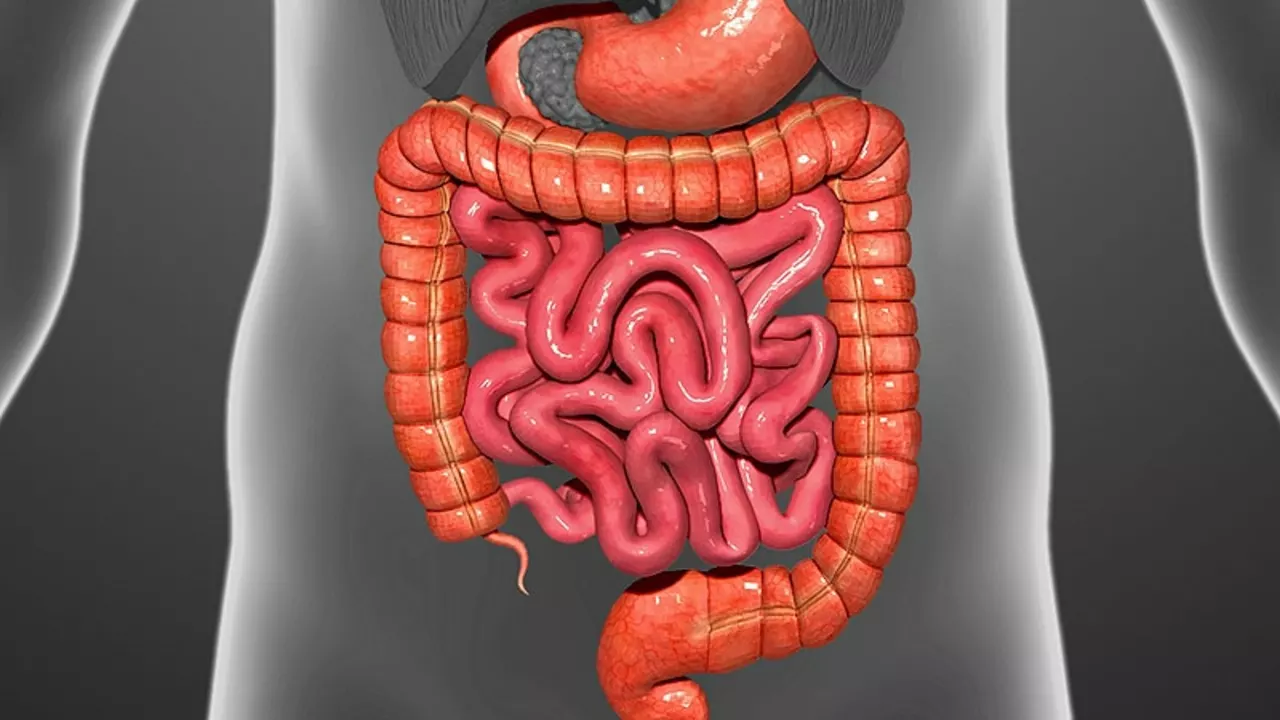
Before we delve into the relationship between Functional Dyspepsia (FD) and Irritable Bowel Syndrome (IBS), it is essential to understand these two disorders. FD is a chronic disorder of the digestive tract characterized by discomfort or pain in the upper part of the stomach. On the other hand, IBS is a common disorder affecting the large intestine, causing symptoms such as cramping, abdominal pain, bloating, gas, and diarrhea or constipation.
Identifying the Symptoms of Functional Dyspepsia and Irritable Bowel Syndrome
Recognizing the symptoms of both FD and IBS is crucial for diagnosis and treatment. While symptoms can vary individually, common signs of FD include bloating, belching, nausea, and a burning sensation in the stomach. IBS symptoms often include abdominal pain, bloating, diarrhea, or constipation, and sometimes even alternating between the two. It's important to note that these symptoms can overlap, which can sometimes lead to confusion in diagnosing these conditions.
Prevalence and Overlap of Functional Dyspepsia and Irritable Bowel Syndrome
It's not uncommon for individuals to suffer from both FD and IBS. Numerous studies have indicated a significant overlap between these two disorders. This overlap suggests a potential common underlying pathophysiological mechanism. It also underlines the importance of understanding the link between these two disorders for accurate diagnosis and effective treatment.
Exploring the Common Causes and Triggers
Although the exact causes of FD and IBS are not fully understood, they are believed to be triggered by similar factors. These may include altered gut motility, heightened sensitivity to abdominal pain, and psychological factors such as stress and anxiety. Additionally, both conditions can be exacerbated by certain foods, suggesting a potential link between diet and these disorders.
Investigating the Role of Gut Microbiota
Emerging research suggests that gut microbiota, the community of microorganisms living in our intestines, may play a crucial role in both FD and IBS. Dysbiosis, or imbalance in the gut microbiota, has been linked to the pathophysiology of both these disorders. This shared factor further strengthens the connection between FD and IBS.
Psychological Factors and Their Impact
There is increasing recognition of the role of psychological factors in both FD and IBS. Stress, anxiety, and depression are often reported by individuals suffering from these disorders. This highlights the role of the brain-gut axis, a complex system involving direct and indirect communication between the central nervous system and the gastrointestinal tract.
Diagnostic Challenges and Approaches
Due to the overlap in symptoms and common triggers, diagnosing FD and IBS can be challenging. The Rome Criteria, a set of symptoms used for diagnosis, is commonly used for both disorders. However, it's important for healthcare professionals to consider the possibility of both conditions in patients presenting with upper and lower gastrointestinal symptoms.
Treatment Options and Management Strategies
While there is currently no cure for FD or IBS, several treatment options and management strategies can help alleviate symptoms and improve quality of life. These may include dietary modifications, stress management techniques, and medications to regulate gut motility and reduce pain. Personalized treatment plans considering the overlap and interaction between FD and IBS can be more effective in managing these conditions.
Conclusion: The Need for Further Research
While the link between FD and IBS is becoming increasingly evident, more research is needed to fully understand the underlying mechanisms and develop more effective treatment strategies. By gaining a better understanding of these disorders, we can improve diagnosis, treatment, and ultimately the quality of life for those living with FD and IBS.
Oh great, another article pretending the gut is some mystical playground. The supposed ‘link’ between FD and IBS is just a flimsy excuse for doctors to sell more meds. Most people can manage their symptoms with simple lifestyle tweaks; we don’t need a fancy research paper every week. Stop glorifying misery and start looking at real solutions.
Honestly this read feels like a lazy remix of every other gut‑health post out there. They toss arond terms like ‘dysbiosis’ and ‘brain‑gut axis’ without even a proper explanation – like we’re supposed to just nod. And the diet advice? Same old “avoid spicy foods” nonsense. It's like they copy‑paste from a textbook and hope nobody notices.
The interplay between functional dyspepsia and irritable bowel syndrome indeed warrants careful consideration.
Current literature suggests that visceral hypersensitivity and dysregulated gut motility serve as common pathophysiological substrates.
Moreover, alterations in the microbiome may potentiate symptom overlap, as demonstrated by recent metagenomic analyses.
Clinicians are encouraged to employ the Rome IV criteria while remaining vigilant for co‑occurring presentations, thereby facilitating a more nuanced therapeutic strategy.
Let me tell you why this whole FD‑IBS connection story is the blockbuster drama of gastroenterology 🎬. First, the researchers love to parade a cascade of scientific buzzwords that sound impressive, such as ‘visceral hypersensitivity’, ‘microbial dysbiosis’, and the ever‑mysterious ‘brain‑gut axis’. Second, they conveniently ignore the simple truth that many patients feel better just by swapping a latte for a glass of water. Third, the supposed ‘overlap’ is often blown out of proportion, turning a modest correlation into a headline‑grabbing myth. Fourth, the pharmaceutical industry sees this as a golden ticket, pushing poly‑pharmacy regimens that promise relief but deliver side‑effects. Fifth, dietitians get dragged into the fray, handing out restrictive meal plans that leave people miserable and hungry. Sixth, anxiety factor is real; telling patients they have two chronic conditions can amplify stress, which in turn worsens gut function. Seventh, the gut microbiome is indeed a fascinating frontier, yet we are still mapping a terra incognita with more questions than answers. Eighth, while some probiotic trials show modest benefits, others reveal no difference from placebo, making the hype look like a roller coaster ride 🎢. Ninth, we must remember that lifestyle interventions-regular exercise, adequate sleep, and mindful eating-remain the cornerstone of management. Tenth, the Rome IV criteria are useful, but clinicians should not become slavishly dependent on checklists, lest they miss the human story behind the symptoms. Eleventh, patient education is paramount; empowering individuals with knowledge reduces the allure of quick‑fix pills. Twelfth, interdisciplinary collaboration between gastroenterologists, psychologists, and nutritionists can break the silo‑mental barrier that fuels confusion. Thirteenth, insurance companies love the diagnostic ambiguity because it justifies endless billing cycles. Fourteenth, the media loves sensationalism, turning a nuanced discussion into click‑bait sensational headlines that mislead the public. Finally, if we strip away the drama, the reality is simple: a personalized, evidence‑based approach is the only path forward, and that’s the story that truly matters 🌟.
Wow groundbreaking insight about spicy food advice
If you’re juggling both FD and IBS, try a step‑by‑step plan: start with a low‑FODMAP trial for two weeks, keep a symptom diary, and gradually re‑introduce foods while monitoring how you feel. Pair this with gentle mindfulness exercises to keep stress in check, and don’t be afraid to ask your doctor about prokinetic options if motility remains an issue. Remember, consistency beats perfection, so stick with the routine and adjust as needed.
Okay so the whole ‘gut‑brain’ conspiracy is just another excuse for diet fads that promise miracles but deliver nada. They talk about ‘micro‑flora’ like it’s some alien invasion, yet the science is still blurry. Honestly, I’d rather trust my grandma’s chicken soup than any over‑hyped supplement they keep screaming about on junk ads.
It’s interesting how different cultures address stomach issues – think of Ayurvedic ginger tonics in India, kimchi fermentation practices in Korea, and the Mediterranean emphasis on olive oil and fresh vegetables. These traditional approaches often align with modern findings on microbiota modulation, suggesting that ancient wisdom might hold clues for managing FD‑IBS overlap. Exploring these dietary patterns could enrich our therapeutic toolbox beyond the usual Western pharmacology.
Sure, the ‘research community’ is just out there trying to help, not secretly gathering our gut data to sell to big pharma for profit. The endless focus on microbiome sequencing is probably a cover for mapping the human body like a surveillance net. And the next thing you know, they’ll be prescribing probiotics that double as micro‑chips.
I totally agree that a multidisciplinary approach is the way forward for patients dealing with both functional dyspepsia and irritable bowel syndrome. First, gastroenterologists can provide the critical medical assessment and rule out any organic pathology that might masquerade as functional disease. Second, dietitians bring valuable expertise in tailoring low‑FODMAP or other therapeutic diets that respect individual tolerances. Third, mental health professionals can address the anxiety and depressive components that often exacerbate gut symptoms, using CBT or mindfulness techniques. Fourth, primary care physicians serve as the central hub, coordinating referrals and ensuring continuity of care. Fifth, pharmacists can assist with medication management, especially when patients are on multiple agents for motility, pain, or acid suppression. Sixth, patient support groups empower individuals by sharing experiences, tips, and encouragement, which can boost adherence to treatment plans. Seventh, researchers should continue investigating the gut‑brain axis, as emerging data on vagal nerve modulation could open new therapeutic avenues. Eighth, health insurers need to recognize the cost‑effectiveness of comprehensive care models, which may reduce emergency visits and hospitalizations. Ninth, technology platforms offering symptom tracking apps can provide real‑time data to clinicians, enabling timely adjustments. Finally, we all must stay humble and remember that each patient’s journey is unique, requiring flexibility and compassion. Let’s keep the conversation alive and push for policies that support integrated care pathways for these often‑overlapping conditions.
Hey there, just wanted to jump in and say that while the article covers the basics, it totally skips over the power of peppermint oil capsules for FD relief – they’re a game changer for many folks I know. Also, don’t forget that low‑dose tricyclic antidepressants can smooth out IBS pain when diet alone falls short. Hope that adds a few useful nuggets to the discussion!
It’s alarming how often the medical community sugar‑coats the reality of chronic gut disorders, painting them as merely ‘inconveniences’ while ignoring the profound impact on patients’ lives. The laziness of repeating the same outdated guidelines without demanding rigorous, patient‑centered research is a disservice. We must call out this complacency and demand higher standards of evidence before we continue to treat suffering as optional.