Understanding Ocular Hypertension and Retinal Detachment
Ocular hypertension (OHT) and retinal detachment (RD) are two prevalent eye conditions that can significantly impact an individual's vision and overall ocular health. Before delving into their relationship, it is essential to understand each condition's basics. Ocular hypertension is a condition where the intraocular pressure (IOP) is consistently higher than normal, potentially increasing the risk of developing glaucoma. On the other hand, retinal detachment is a serious eye emergency characterized by the separation of the retina from its underlying tissue, potentially leading to vision loss. In this article, we will explore the relationship between these two conditions and the significance of early detection and intervention.
Factors Contributing to Ocular Hypertension
Various factors contribute to the development of ocular hypertension. Some of the most common causes include the excessive production of aqueous humor, reduced drainage of the aqueous humor through the trabecular meshwork, and the use of certain medications, such as corticosteroids. Age, ethnicity, family history, and certain medical conditions, such as diabetes and hypertension, are also known to increase the risk of developing OHT. Understanding these risk factors is crucial in determining the likelihood of developing ocular hypertension and the potential for retinal detachment.
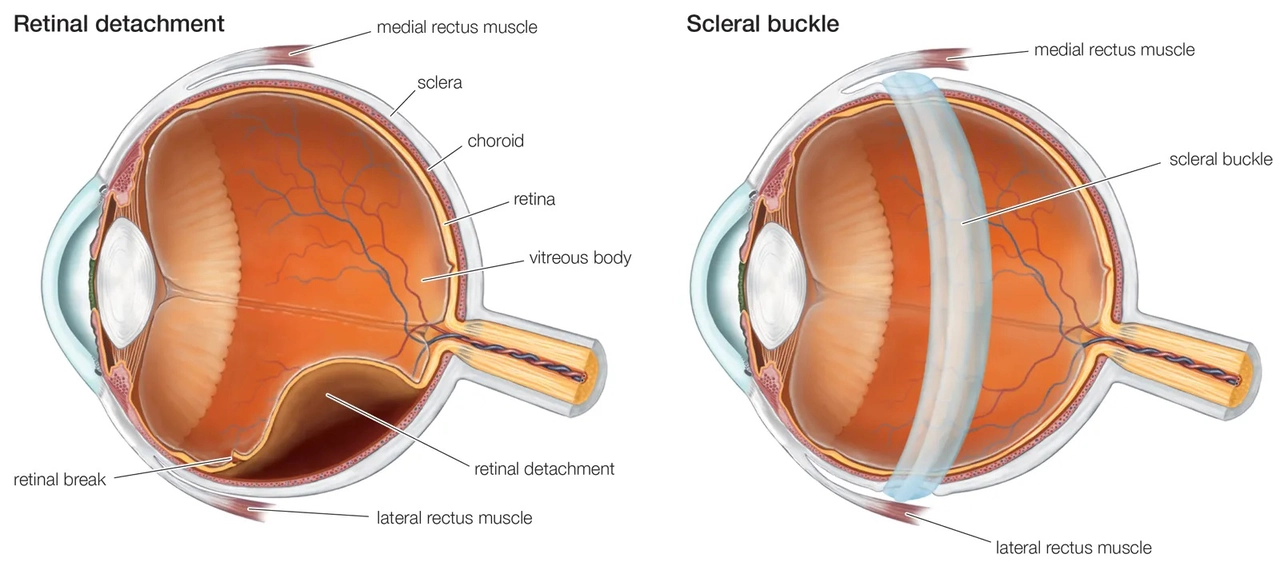
How Retinal Detachment Occurs
Retinal detachment can occur through various mechanisms, such as a tear or hole in the retina, traction from vitreous or scar tissue, or fluid accumulation beneath the retina. Factors that increase the risk of retinal detachment include aging, trauma, high myopia (nearsightedness), previous eye surgery, and family history. While the exact relationship between OHT and RD is not entirely understood, it is believed that increased intraocular pressure may exacerbate the risk factors associated with retinal detachment, leading to a higher likelihood of developing this severe eye condition.
Ocular Hypertension as a Potential Risk Factor for Retinal Detachment
Several studies have explored the relationship between ocular hypertension and retinal detachment. While some studies suggest a potential association between increased intraocular pressure and the development of retinal detachment, others have found no significant link. The relationship between these two eye conditions is complex and may vary depending on individual risk factors and the presence of other eye conditions. However, it is crucial to monitor and manage ocular hypertension to minimize the potential risks associated with elevated intraocular pressure, including retinal detachment.
Importance of Early Detection and Intervention
Early detection and intervention in both ocular hypertension and retinal detachment are critical in preserving vision and maintaining overall ocular health. Regular eye examinations, including IOP measurements and fundus examinations, can help identify signs of ocular hypertension and retinal detachment in their early stages. Timely intervention, such as the use of intraocular pressure-lowering medications or surgical procedures for retinal detachment, can significantly improve the prognosis and reduce the risk of vision loss. It is essential for individuals at risk for these conditions to maintain regular eye care appointments and promptly report any sudden changes in vision or eye-related concerns to their eye care professional.
Treatment Options for Ocular Hypertension and Retinal Detachment
Various treatment options are available for managing ocular hypertension and retinal detachment, depending on the severity of the condition and the patient's individual needs. For ocular hypertension, treatment may include the use of IOP-lowering medications, laser procedures, or surgical interventions, depending on the patient's response to treatment and the risk of developing glaucoma. In the case of retinal detachment, surgical procedures such as vitrectomy, scleral buckle, or pneumatic retinopexy may be recommended to reattach the retina and preserve vision. Prompt treatment and close monitoring of these conditions are vital in ensuring the best possible outcome.
Conclusion: The Complex Relationship Between Ocular Hypertension and Retinal Detachment
In conclusion, the relationship between ocular hypertension and retinal detachment is complex and not entirely understood. While some studies suggest a potential association between these two eye conditions, others have found no significant link. However, given the serious nature of both ocular hypertension and retinal detachment, it is crucial to closely monitor and manage these conditions to minimize the risks associated with elevated intraocular pressure and retinal detachment. Early detection, intervention, and appropriate treatment are vital in preserving vision and maintaining overall ocular health.
Listen up, folks-this whole oculr hypertension thing is not just a minor inconvenience, it’s a looming disaster waiting to strike! If we keep ignoring the sky‑high pressure in our eyes, we’re basically signing a death certificate for our own vision. The medical community has been waving red flags for years, yet people still act like it’s just a “little ache.” Wake up and get those check‑ups before it’s too late!
What the elite don’t want you to know is that ocular hypertension is part of the globalist “control‑the‑population” agenda. They pump steroids into the market, hoping to raise intra‑ocular pressure across the nation, while the mainstream media pretends it’s just a “eye thing.” As proud Americans we must resist this medical manipulation and demand transparent research before any more eyes are compromised.
Hey everyone, just wanted to share that regular eye exams are the MVPs in catching both OHT and potential retinal detachment early. A full dilated exam can reveal subtle changes before they become sight‑threatening. If you have a family history of glaucoma or high myopia, schedule a check‑up now; early intervention can save a lot of hassle later. Stay proactive and keep those eyes happy!
It is, without exaggeration, a remarkable feat of modern ophthalmology that we find ourselves debating whether elevated intra‑ocular pressure might subtly predispose one to retinal detachment.
One might imagine that Nature, in its infinite wisdom, would simply keep these mechanisms neatly compartmentalized, yet the literature suggests a more tangled web.
Some studies, perhaps too eager for headlines, hint at a correlation, while others steadfastly deny any substantive link.
The methodological heterogeneity across these investigations leaves the discerning clinician in a state of bemusement.
One could argue that the statistical power of these trials is insufficient to draw any definitive conclusions.
Conversely, the counter‑argument posits that the absence of evidence is not evidence of absence, a philosophical maxim that delights epidemiologists.
Moreover, the pathophysiological plausibility, involving vitreoretinal traction exacerbated by chronic pressure fluctuations, cannot be dismissed outright.
Yet, the clinical reality remains that most patients with ocular hypertension never develop a retinal tear.
In practice, we continue to monitor IOP diligently, employing prostaglandin analogues or laser trabeculoplasty as needed.
Simultaneously, we educate patients about the classic warning signs of detachment: flashes, floaters, and a curtain‑like shadow.
It is, of course, a delicate balance between over‑medicalization and prudent vigilance.
The economic implications of blanket screening programs also merit rigorous cost‑benefit analysis.
Ultimately, the decision to intensify surveillance should be individualized, taking into account age, myopic degree, and past ocular trauma.
While the jury may still be out on a direct causal relationship, the prudent clinician errs on the side of caution.
In summary, the interplay between ocular hypertension and retinal detachment remains an intriguing, albeit unresolved, chapter in our collective understanding.
Imagine the eye as a delicate canvas, where elevated pressure paints a subtle, unsettling shadow that could, under the right circumstances, coax the retina away from its masterpiece. While I’m not prone to dramatics, I find the analogy vivid enough to remind us of the stakes involved.
Philosophically speaking, one might ponder whether the pressure within our eyes is a metaphor for the pressures we place upon ourselves in life-an endless cycle of tension and release. Yet, I’ll be honest, I haven’t read the full meta‑analysis, so I’ll just say, “meh, sounds interesting, maybe worth a glance.”
From a contrarian perspective, the prevailing narrative that ocular hypertension directly augments retinal detachment risk is, frankly, a textbook case of confirmation bias. The empirical data, when stripped of its sensationalist veneer, reveal a paucity of robust, longitudinal evidence. In other words, we should recalibrate our clinical heuristics and demand stratified cohort analyses before endorsing any causal inference.
Let us consider, for a moment, the multifactorial etiology of ocular hypertension-genetic predisposition, aqueous humour dynamics, systemic comorbidities-, and juxtapose this with the complex biomechanics of retinal adhesion; ; ; the literature, whilst extensive, remains inconclusive, thus urging a measured, evidence‑based approach, rather than precipitous clinical extrapolation.
Agree, vigilance is key. Regular screenings can help us stay ahead, regardless of any broader agenda.
Wow, thank you for that exhaustive dissertation-clearly, we’ll all need a PhD in ophthalmic jurisprudence before we can schedule a simple eye exam. Your prose is as enlightening as a fluorescent bulb in a blackout.
Honestly, the drama feels a bit over‑the‑top 🤦♂️, but the warning isn’t lost on me. The ‘red flags’ are indeed there, and the ocular pressure can be a silent threat. Stay alert, folks! 👀
Sure, regular check‑ups are “MVPs,” but who’s to say the doctors aren’t in on the big pharma scheme? I mean, they love selling drops, right? Probably just another way to keep us compliant.
Appreciate the philosophical take! Even if the evidence is thin, staying informed never hurts. Keep those eyes on the prize :)
Love the canvas metaphor, Gary! It really paints the picture of why we shouldn’t ignore pressure spikes. Let’s all champion early detection and share this knowledge.
Honestly, this whole debate is just eye‑candy for the media.
i cant help but wonder if we r all just chasin shadows, thinkin the flashes are real when maybe they r just our mind playin tricks, but hey, that's the kinda deep stuff that keeps the convo goin.