When you pick up a prescription, do you ever check the label and wonder if the generic version is really the same as the brand-name drug you used to take? You’re not alone. Even though generic medications make up 90% of all prescriptions filled in the U.S., nearly one in three patients still believe they’re less effective. And the reason isn’t science - it’s stories.
Online reviews, forum posts, and personal anecdotes are shaping how people feel about generics more than any FDA brochure ever could. A Reddit user named u/ChronicPainWarrior wrote in March 2023: "My doctor switched me to generic Lyrica and within two weeks my nerve pain returned-I’m convinced the generics aren’t made to the same standards." That single comment reflects a pattern seen across thousands of posts. On PatientsLikeMe and r/pharmacy, nearly half of all generic-related discussions mention "different side effects" or "not working as well." Meanwhile, others share wins: "After 3 years on generic sertraline, I’ve saved $2,180 with zero difference." These voices don’t just echo - they change behavior.
What Exactly Is a Generic Drug?
A generic drug isn’t a knockoff. It’s the exact same medicine, chemically speaking. The active ingredient - the part that actually treats your condition - must match the brand-name version down to the last molecule. The FDA requires this. But here’s where things get tricky: the inactive ingredients can be different. That means the color, shape, fillers, or coating might change. For most people, that’s harmless. For some, it’s enough to trigger a psychological reaction.
Take bioequivalence: the gold standard for generic approval. To be approved, a generic must deliver between 80% and 125% of the brand’s drug concentration in the bloodstream. That’s not a wide range - it’s tight enough to ensure real therapeutic equivalence. For drugs with a narrow therapeutic index - like warfarin or levothyroxine - the standard is even stricter: 90% to 111%. These aren’t guesses. They’re backed by clinical trials. Yet patients don’t hear this. They see a cheaper pill and assume it’s cut corners.
The Psychology Behind the Doubt
It’s not just about pills. It’s about perception. The mind doesn’t always follow data. If a pill costs 85% less, the brain says: "This can’t be as good." That’s called the nocebo effect - the opposite of placebo. When you expect side effects, you’re more likely to feel them. Studies show patients who think they’re taking a generic report 27.4% more side effects than those who think they’re on the brand - even when both are identical.
And it’s not just patients. A 2015 review of 52 studies found that 35.6% of laypeople believe generics are less effective. Doctors? 28.7%. Pharmacists? 23.6%. The gap is real. And it’s growing because of what people read online. A 2024 machine learning analysis of 6,012 forum posts found that "cheap and poor copy" was the third strongest predictor of rejection. Meanwhile, "recognizing generics as equivalent" was the strongest predictor of acceptance.
How Online Reviews Change Behavior
Let’s look at real numbers. In a 2018 European study, patients were given identical tramadol pills - one group got them in branded packaging, the other in generic packaging. The group that thought they were getting the brand completed 77.3% of their 7-day course. The group who thought they were on generics? Only 54.6%. That’s a 22.7% drop in adherence. They also reported 15.6% higher pain levels - even though the medicine was the same.
Online reviews amplify this. When someone writes, "Generic X didn’t work for me," it’s not just one story. It’s a signal. Algorithms push it to others with similar conditions. Someone scrolling through forums looking for help with anxiety sees ten posts saying "generic sertraline made me feel worse" - and ignores the two saying "it saved me $200 a month." That’s how perceptions become reality.
Who Influences Patients Most?
Here’s the good news: the people who can fix this are already in the room. Healthcare providers. A 2020 study found that 69.8% of patients were more likely to accept a generic if their doctor or pharmacist recommended it. That’s not because providers are persuasive. It’s because they’re trusted.
But here’s the problem: most don’t talk about it. The average primary care visit has just 1.7 minutes for medication discussions. Pharmacists, who have more time, often skip the explanation entirely. Yet when they do speak up - even for 90 seconds - patient acceptance jumps by 38.7%. One pharmacy chain in California trained staff to say: "This generic has the same active ingredient as your old pill. The FDA checks it just as closely. The only difference? You’re saving $120 this month." Within six months, patient questions about generics dropped by over half.
What Works: Real Solutions
Some health systems are already fixing this. Kaiser Permanente started handing out simple one-page fact sheets titled "Generic Medication Facts." It lists: what’s the same, what’s different, why it’s safe, and how much you save. Within six months, adherence rose by 18.6%. No fancy tech. Just clear words.
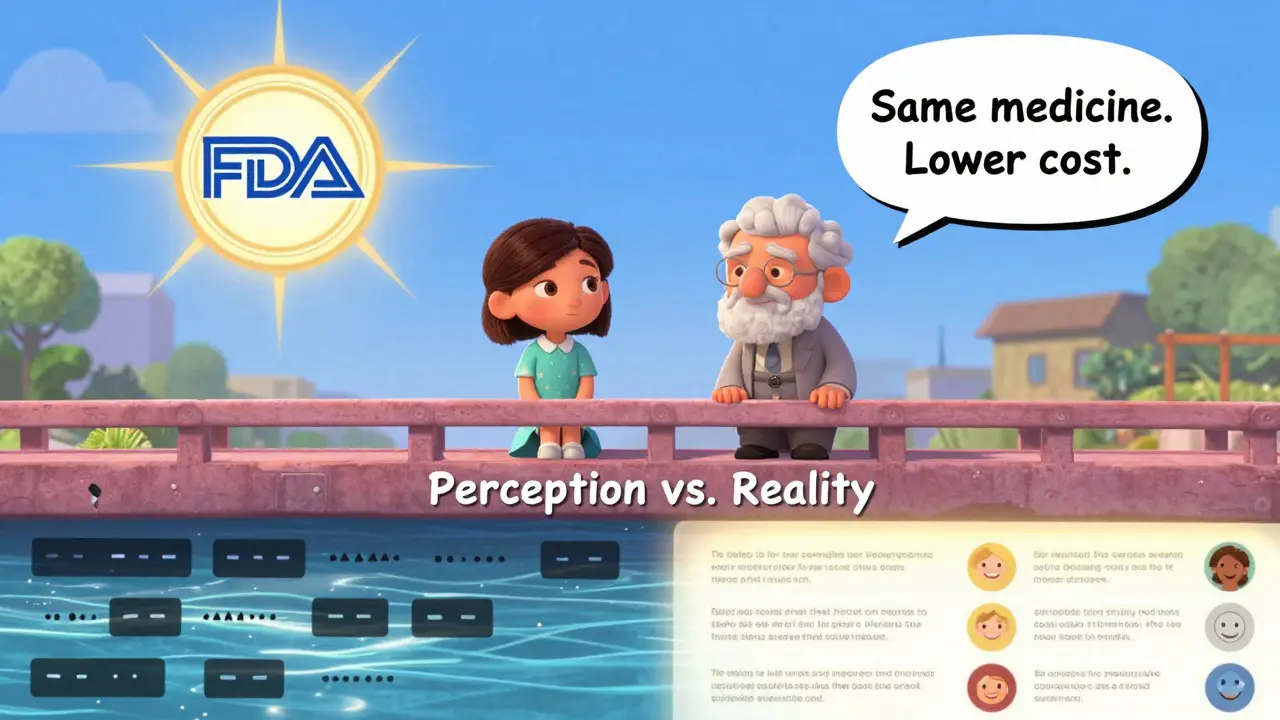
The FDA’s new "Generics: Same Medicine, Lower Cost" campaign is also showing results. After six months, consumer confidence improved by 22.4%. They’re using real patient stories - not just data - to rebuild trust.
And there’s a new trend: authorized generics. These are brand-name drugs sold without the brand logo - same factory, same formula, just cheaper. In Q4 2023, prescriptions for these jumped 37.6% year-over-year. Patients trust them because they know who made them.
Who’s Most at Risk?
Not everyone feels the same way. Younger patients - those under 35 - are twice as likely to trust generics as those over 65. Education matters too. People with higher education levels understand bioequivalence far better. And it’s not just about money. Patients who’ve had bad experiences with brand-name drugs - maybe they had side effects or couldn’t afford them - are more open to generics. But those who’ve never had a problem? They stick with what they know.
What’s Next?
Technology is stepping in. AI models can now predict which patients are likely to reject generics based on age, income, and past behavior. One study using XGBoost hit 89.1% accuracy. That means clinics can target outreach before the first prescription is filled. Blockchain is being tested too - to prove a pill’s origin. If you can scan a code and see exactly where your generic was made, trust grows.
But the real fix isn’t tech. It’s conversation. Every time a pharmacist says, "This is the same medicine, just cheaper," they’re doing more than selling a pill. They’re changing a belief. Every time a doctor explains why the FDA requires identical active ingredients, they’re countering a myth.
The data is clear: generics work. They’re safe. They’re effective. But numbers don’t change minds - stories do. And right now, too many stories are negative. It’s time to make sure the real ones get heard.


